By Amin H. Karim MD
In 1993, I worked at a small hospital called the Del Oro Hospital, which was established by a group of physicians in the Texas Medical Center who wanted to create a hospital outside the domain of the major players of the Texas Medical Center. It was a 100 bed hospital located on Greenbriar Avenue next to the Reliant Stadium (now called NRG Stadium). The hospital was later sold to Hospital Corporation of America (HCA) and later to Columbia Hospital and then back to HCA when Columbia went bankrupt. The Texas Women’s Hospital is behind this hospital. The hospital closed in 1995 and was torn down. It is now replaced by an extension of the Women’s Hospital.
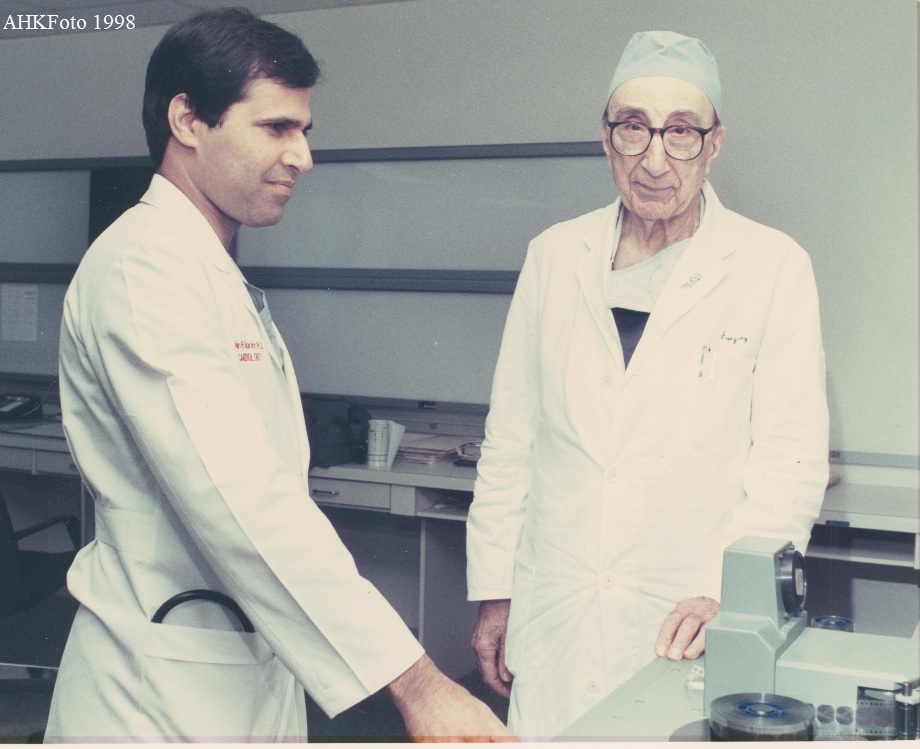
Late Dr. Pedro Rubio was a cardiovascular surgeon trained by late Dr. Michael E. DeBakey at Baylor College of Medicine. He was the only CV surgeon at De Oro for a long time. He had an freak accident at home when he tripped and injured his elbow; he retired thereafter and later passed away (may he Rest in Peace). Dr. Rubio and I saw a case which is described in this paper and turned out to be interesting and unique enough for us to report it in literature. (Amin H. Karim November 24 2023)
Month: November 2023
Coronary Spasm During Thrombolysis.
By Amin H. Karim MD
An article published in the Texas Heart Institute Journal in 1988 after the TIMI Trial 1 had been completed and the standard of care for acute myocardial infarction was thrombolysis with Tissue Plasminogen Activator. (TPA) made by Genentec. We wrote this article as fellows of the Baylor College of Medicine, Houston, Texas. (AHK November 24 2023)
American College of Physicians
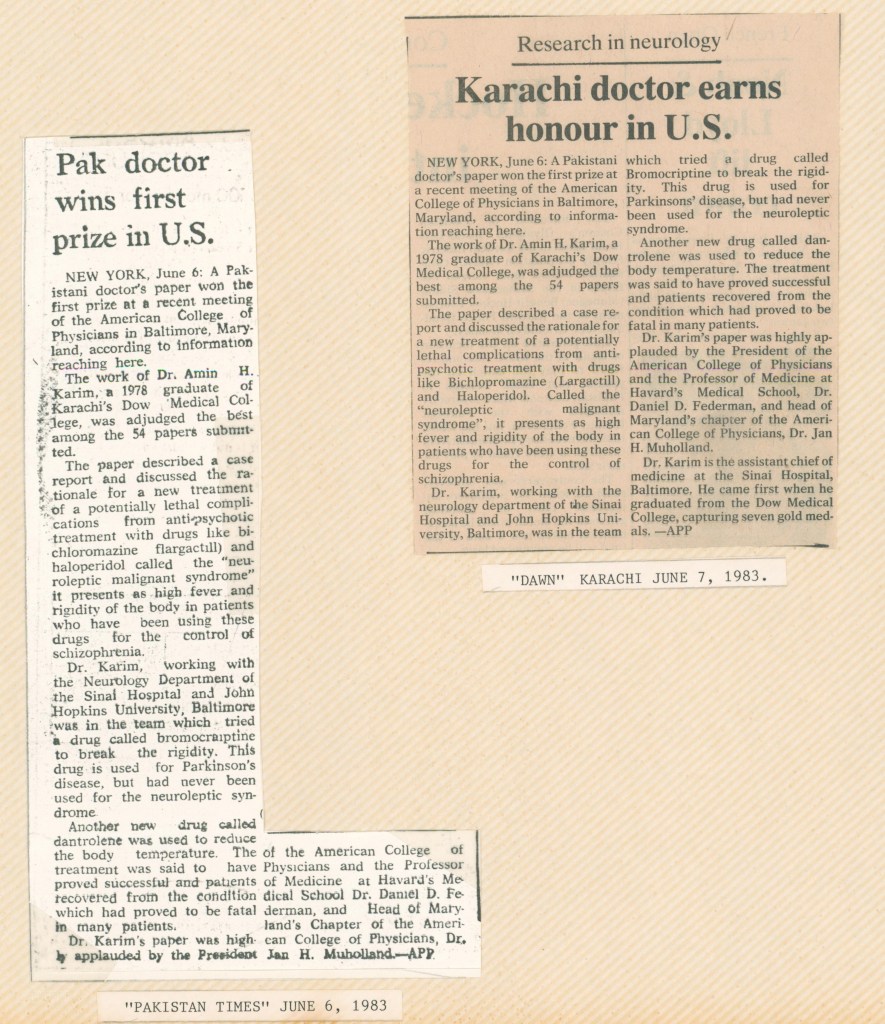
Answering the Call
By Amin H. Karim MD
It was a late autumn night with typical torrential Houston rain, and I was on call for the ST eleva‐ tion myocardial infarction (STEMI) team, which consists of an interventional cardiologist, a traineefellow, a cath lab registered nurse, and cath lab and radiology technicians. It was 3:30 AM and Iwas deep in sleep, only vaguely aware of my beeper going off and quite unaware of the storm out‐ side. The emergency room (ER) physician wanted my opinion on an electrocardiogram (EKG) of apatient with chest pain to see if it qualified as an acute myocardial infarction. He texted the EKGimage to my mobile phone, and I staggered to the closet to turn on the light and read it. I relayedthat I was not impressed at the degree of ST elevation, he concurred, and I sank back into bed. Awhile later, the ER physician called again with a repeat EKG, this time with more ST elevation andan elevated serum troponin level. Hastily, I slipped into my scrubs and quietly tiptoed to avoidwaking my wife.
Rain pelted my car as I drove through the neighborhood in utter darkness. Within a few blocks, Inoticed that the water level had risen but couldn’t gauge how high—simply because there were noother cars or street signs for comparison. I slowly slogged through, only to find my car splutteringbefore eventually stopping completely. It restarted just long enough to hobble to a slightly lessflooded spot on the main road, where it completely died, the dreaded engine warning light flash‐ ing on the dashboard.
I started to sweat as the gravity of the situation took hold. The patient was probably in the cardiaccath lab by now, and the cardiologists’ guiding principle, “time is muscle,” ran through my head:The longer it took to open the vessel, the more myocardial damage. I looked around and the streetwas desolate. The hospital was a good 3 miles away, and the road ahead looked flooded. Walkingwould mean wading through the water with its attendant dangers of electrical wires and the like.
Wade back to my house?
I thought. Only a few blocks away, this seemed like the logical option.
Call the ER physician and tell him to treat the patient with a thrombolytic drug?
Since thrombolytictherapy is the second-best way to treat an acute myocardial infarction, this was another sound op‐ tion, albeit one that does not always work.
Call 911?
And tell them what?
Suddenly, the solution popped into my head: Uber! Although I had never used it, the app was onmy iPhone. I signed in, entered my location and the hospital address, and sure enough there was adriver on the freeway just minutes away. The cost, of course, would be double. I watched the appas it traced the car coming towards me. After getting in, I directed the driver through a route thatis usually not flooded. Remarkably, I made it to the cath lab before the rest of the team, and wewere able to perform the procedure under the mandatory 90-minute door-to-balloon time. Thepatient did well, and as I breathed a sigh of relief, I remembered that there was still one morething to tackle.
For the second time that night, I called Uber. The driver dropped me off at my car, where I thencalled a wrecker. My car had sucked up water and blown a hole in the engine, but the wreckerdriver refused to give me a tow until I gave him cash, which required another trip to the ATM ma‐ chine. After a month of haggling with the car dealership and insurance company, I finally had theengine replaced at a cost of several thousand dollars, and I was back in business.
While in the midst of this ordeal, I felt some regret at being an interventional cardiologist with itsnecessary obligations to care for patients in acute situations. Yet after the procedure, I felt gratefulfor being able to use my skills to save heart muscle and, potentially, a life. Still, I resolved to resignfrom the STEMI call schedule the following year, feeling too old (or maybe too tired) for all thisexcitement.
The next year, however, I found myself signing up for twice as many calls. I guess for some die-hard physicians,
chronic workalcholism and patient dedication are incurable conditions!
PUBLISHED IN THE METHODIST DEBAKEY CARDIOVASCULAR JOURNAL Methodist Debakey Cardiovasc J. 2019 Apr-Jun; 15(2): e1. doi:
10.14797/mdcj-15-2-e1 PMCID: PMC6668749 PMID: 31384387
Varied Groups and Websites by AHK
Here are some groups on FaceBook which I have started from time to time and are still going strong. You are cordially invited to join them if you have interest or if you satisfy the criteria, as some of them are restricted to particular alumni. Most of the groups are on auto pilot and need little maintenance.
A) FACEBOOK GROUPS:
a) GlobeMedic This comprises physicians and health care professionals of Pakistan origin settled all over the Globe.
b) HoustonDocs This is restricted to health care professionals of Pakistan origin living in the Greater Houston area.
c) LikeMind for Muslims living in North America
d) Pak Americans open to all Pakistanis in North America
e) GlobeCardio for cardiologists of Pakistani origin anywhere.
f) Karachi Past and Present for anyone who loves Karachi.
g) HeartCirclers for health professionals in the Texas Medical Center of Houston.
h) DowList for faculty, alumni and students of Dow University of Health Sciences.
i) StPatsKarachi for alumni of St. Patrick’s High School, Karachi.
j) RealBucks for financial discussions in USA
h)RealtyStars for real estate interchange in USA.
i) HomeLand Politics for US related political discussions.
B) EMAIL GROUPS
a) GlobeMedic@yahoogroups.com for Pakistan Descent physicians
b) HoustonDocs@googlegroups.com for physicians in Houston
c) Heartcirclers@googlegroups.com for physicians in the Texas Medical Center.
d) StPats@googlegroups.com for St. Patrick’s alumni
e) APCNAteam @googlegroups.com for members of the American Association of Pakistan
Descent Physicians of North America (APCNA)
f) DowList@googlegroups.com for Dow Alumni.
g) Dow77study@googlegroups.com for alumni of the Dow Medical College Class of 1977
C) WEBSITES AND BLOGS.
Open to all to visit at your convenience.
In the Lighter Vein 1
WIDOW MAKER LESION
I cath a patient with chest pain today as an emergency. The patient asked: “What did you find, doc?” I said ” I found a narrowing in the big artery that goes to the front of your heart”.
He said: “You mean the widow maker lesion”
I said: “No Sir, it used to be called the widow maker lesion.
Now it called the New Husband Maker Lesion”
It made him laugh.
SICK SINUS SYNDROME:
Today a elderly cardiac patient asked me if the metoprolol he is taking will affect his sick sinus syndrome. I was a bit surprised. I said it certainly can do that and slow the heart rate. He said ” Doc, then I should not be on it!” “But” I said. “How do you know you have sick sinus syndrome?” He remarked: ” I have had sinuses for a long time and I read on the internet that metaprolol should not be taken if you have sick sinuses”
(Amin H. Karim MD)
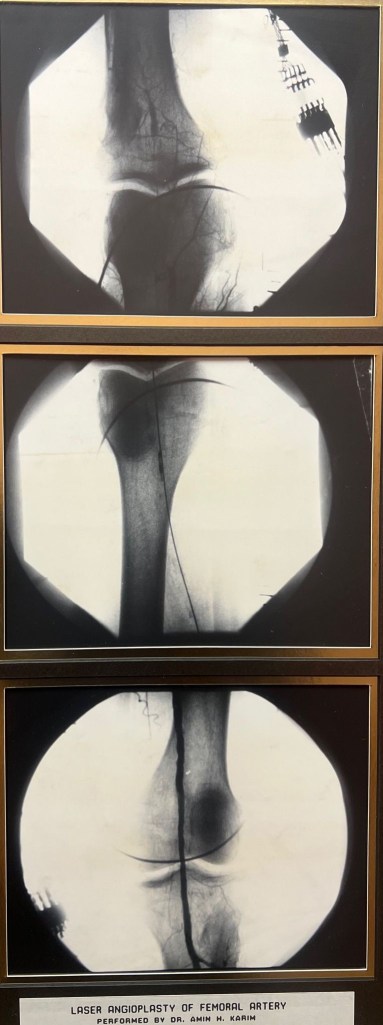
Exhimer Laser Angioplasty of Peripheral Arteries
By Amin H. Karim MD
Interventional friends; here is a piece of history. The year is 1989 ( 34 years ago). Excimer ( short for excited dimer) was approved for peripherals and later coronary use; we, in Houston, were one of the first to try it out after attending a laser safety course. Above is an angioplasty on a CTO of femoral artery. The probe went in ( without wire) like a “knife through butter” followed by wire and balloon ( stents had not been invented yet) of course as expected there was thermal damage to intima and reactive fibrosis and Re stenosis. But did have impact on patient psyche of having “ cutting edge” procedure ( no pun intended).
The author can be reached at globelinker@gmail.com
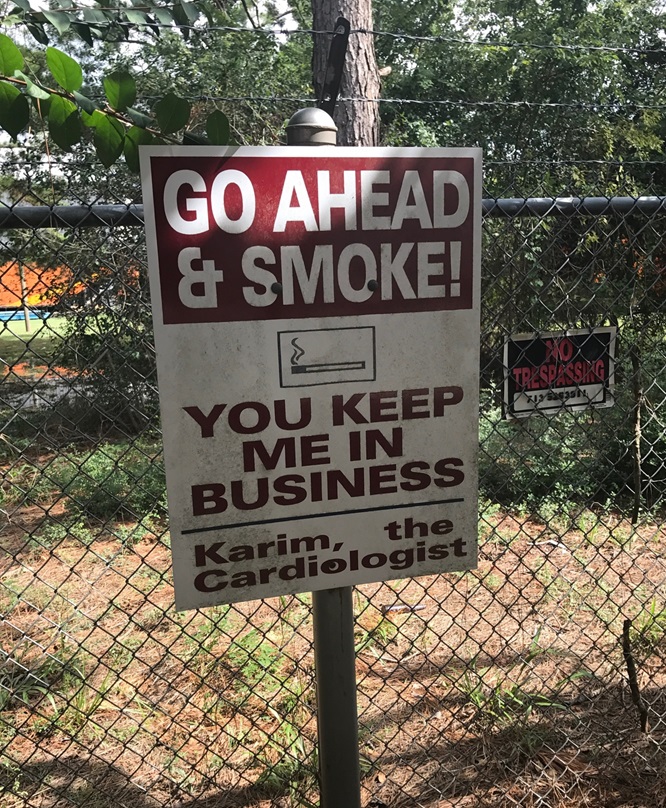
Legendary Surgeons of Houston.
By Amin H. Karim MD
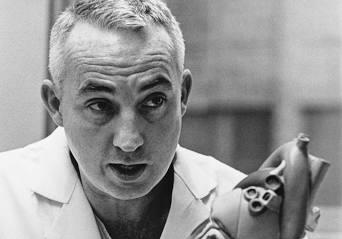
That’s Norman Shumway, the first to perform heart transplant in USA in 1968, after Christian Bernard did the first in the world in 1967. ( I had just graduated from school!) . Unfortunately never met Dr. Shumway, although he may have come to Texas Heart Institute and known Howard Frazier who was into heart transplants in Houston. Shumway died in 2006 of lung cancer. Amazingly, two other legends at Houston Methodist Stanley Crawford, pioneer of aortic aneurysm surgery, and Jimmy Howell, both smokers and both died of lung cancer!. May they all rest in Peace. They gave a lot to humanity. They lived in times when doctors advertised smoking for asthma!
ABOUT Dr. DEBAKEY
It is said as a kid DeBakey who grew up in New Orleans went to the school library and asked the librarian if he could borrow the Encyclopedia Brittanica; the librarian of course told him he cannot since it is a reference. His dad bought a set for him and he read all the volumes cover to cover.
MEDs preferred cardiologist was Dr. Mohammed Attar, a solo like me; he probably liked him because Attar is very good and meticulous and also because his roots are in Syria and Lebanon like Dr DeBakey. Attar and I covered each other for more than 20 years. MED daily rounds would start exactly at 3 pm. He would be walking VIP the stairs with his entourage of Dr Attar, fellows residents behind. One nurse said you guys look like a hen followed by chicken. 🙂 when Attar was out of town I would have to be ready by 3 and know all his patients like an intern! But he was always nice as long as you knew the patients.
Dr. DeBakey had his office on the 9th floor of Fondren Building in Methodist. He had the privilege of holding the fireman’s key to the elevator. When he got in he would use the key and press 9 which means elevator goes straight to 9. One was supposed to leave the elevator regardless and he would ride up. May he rest in Peace.
Some good things about MED ( initials for Michael E. DeBakey) he did open hearts by thousands. Kept a file on each patient. If we Cath his patients later we would have to send a diagram to him. He would carefully record the findings comparing with the ones before and after surgery and write pencil notes. His office was inside the hospital; he stayed on full time faculty of Baylor till the end and never did private practice. Passed away in 2008 at age 99.
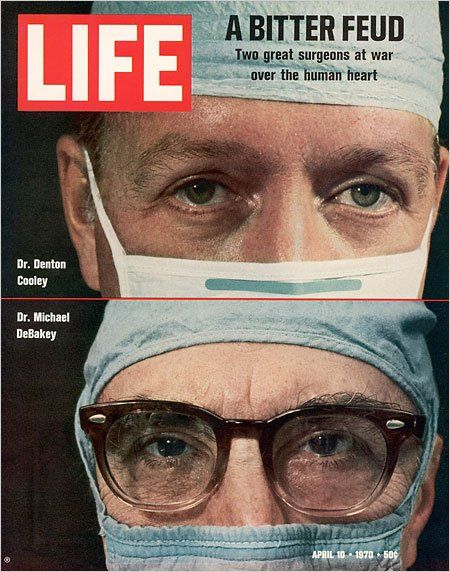
Late Denton Cooley certainly was the more friendly of the two. He held cardiologists close to his heart inviting them to his ranch every year ( Cool Acres Ranch in Rosenberg) for BBQ. He would play softball with the kids he had 5 daughters ( some were surgeons). Cardiologist Virendra Mathur made him famous in India and many came to him including Kishore Kumar, Madam Noor Jehan and others. When General Habibullah ( Gen Ayub Khan’s samdee) who was Mathur’s patient when he found out there was a Pakistani cardiologist next door in Methodist he switched over and he remained my patient till the end; same happened with some others from Pakistan. Later Cooley did not get into newer techniques like mini cab calling them gimmicks.
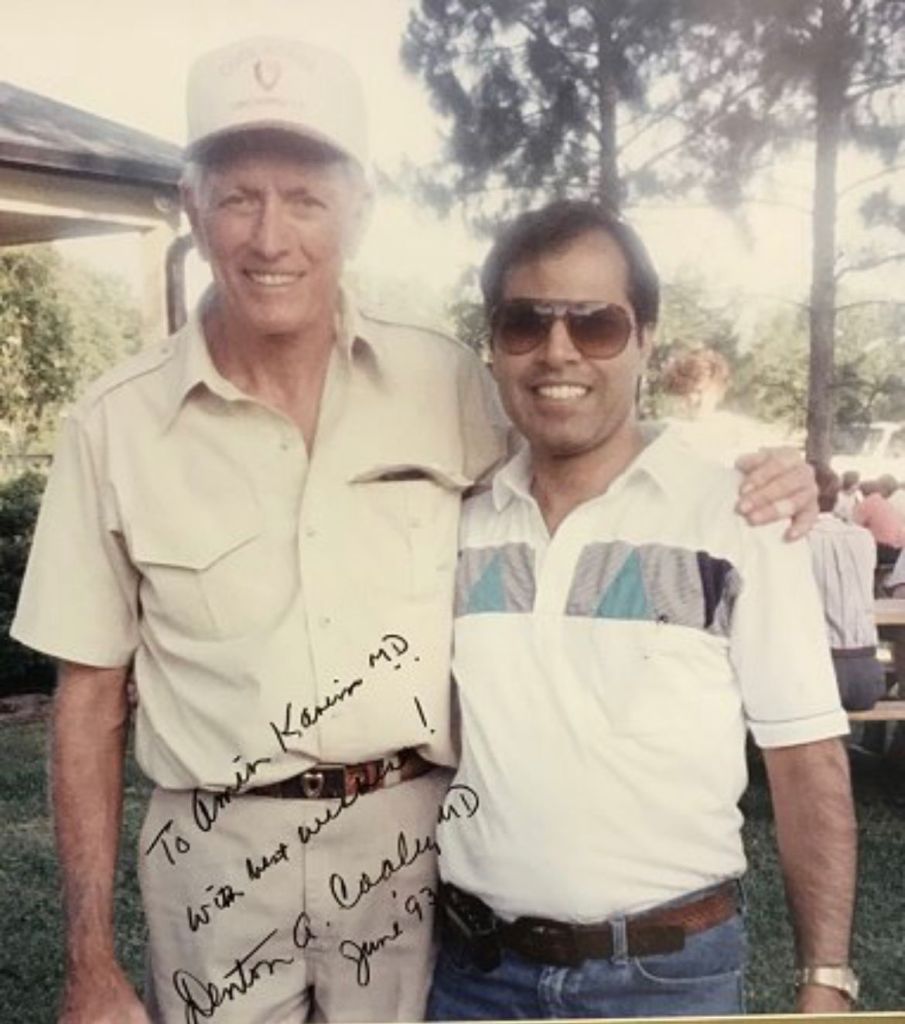
Certainly Naeem as time permits; have seen and worked with both of them over the years and of course heard a lot of Doctors Lounge Talk. I was one if the blokes who was on good terms with both these “ rivals” in two neighboring hospitals. Late Oro dental surgeon Oscar Moldonado and Dr. George Noon would similarly claim!
I will try to keep what I write free of what can even remotely be construed as gossip or back biting (the latter strictly not allowed in Islam). Will write what I saw or others who I trust recounted. Of course, being busy and running to different hospitals to make a living, there was no time to record numbers and stats. etc ( not easily revealed by hospitals anyway). Blogs better than books since they can be updated and read by all for free. History aside, maybe other interventionists will take a hint and start their own blogs and record their interesting cases and how they were treated ( I see some remarkable cases on WhatsApp groups). Later new fellows can benefit from it. WhatsApp and FaceBook messages are fleeting. YouTube can also be used similarly by creating your own channel. Just have to make sure patient ID remains hidden (we know the rules) Youtube is universal and residents all over the globe can benefit. This is all informal, ongoing and individually powered and costs nothing.
Author can be reached at globelinker@gmail.com
The Plump RCA
By Amin H. Karim MD
A 85 year old patient on hemodialysis, presented with acute coronary syndrome. Cath showed a totally occluded RCA. This is just a straight forward case being posted initially to test the website and ease of uploading videos.
Prof. Michael E. DeBakey
PROF. MICHAEL E. DEBAKEY’S ROUNDS 1980 AND BEFORE:
Prof. Michael E. DeBakey is nothing short of a legend of Medicine. He was the Head of Department of Surgery at the Baylor College of Medicine, Houston, Texas.
This write up is not meant to write his bio. He already has books written on him. These are just quiet observations of someone who worked at the Houston Methodist Hospital from 1984 to date and saw and worked with the Professor as a non surgeon and for a limited time.
Prof. DeBakey rounded Monday to Friday starting at 4 PM. He carried a patient load of roudndly 100-120 patients at a time. He was very meticulous and expected to know details on each of his patient. The resident responsible for the patients had to be on his/her feet and expected to know progress, labs, vital signs and report to the Professor. Dr. DeBakey expected all the consultants, some Chiefs of their own departments to accompany him on the rounds so that quick decisions could be made. This included the Cardiologist (sometimes more than one) the Internist, the Nephrologist, Infectious Disease Specialist, Pulmonologist and the like. The attrition rate of residents was about 20% either resigning due to stress and could not take it any more or being fired on the spot.
FONDREN ICU RESIDENT: The Cardiovascular ICU was the location for this famed rotation which all CV residents had to undertake and was one test of nerves and patience. Professor likely used this as The Test to see who could survive his training and come out a trained surgeon. First it was straight 3 months ( as related to me by Dr. Phillipe, Urologist) and later it was changed to 60 days done twice. (related to me by Dr. Hazim Safi, CV Surgeon) During this rotation, the resident LIVED in the ICU and was not allowed to leave till the rotation ended. He/she slept in the isolation room ( no attached bathroom, just a sink) and was on call 24/7. His job was to round on each and every patient in the ICU and write notes, and fill out the detailed labs on each patient to present to the Professor during rounds. In the early days there was a RED LINE which could not be crossed by the resident to go out. (more about this later). Actually less residents were fired from this rotation than on the other rotations, likely because by the time they came to this rotation they had already weathered the “storm”.
PROFESSOR DEBAKEY’S RED LINE:
A red line similar to this one once was at the entrance to the Fondren ICU at the Methodist Hospital, Houston, Texas. It represented the line that could not be crossed by the surgical resident doing his three month rotation in the Cardiovascular Intensive Care Unit. Once the resident entered the Unit he stayed there for the next 3 months, sleeping in a room, working, rounding, writing notes, doing procedures, managing ventilators, admitting and discharging patients, accompanying Prof. DeBakey on rounds once or twice or more daily. There was no timing of rounds which could start and end when all the patients had been seen. Resident ate, drank, prayed, showered, shaved and slept when he could in the Unit. He could see his family once in a while through a small window. One thing he could not do till the last day of his rotation is to cross the red line. For if he did, it would mean an end to his surgical residency and his career. He would be dismissed from the Surgical program and from the Hospital. The following true incident was quoted by a surgeon (who is now a urologist) who actually did this rotation in 1960’s.There was a Philipino resident in the group. He had done 10 weeks of the rotation with 2 weeks more to go.He was excited and out of sheer fun he went near the red line and actually crossed it and bragged to the nearby patient liaison secretary that he had only two more weeks to go and then he would be free. Alas, his excitement was not to last long. The secretary promptly picked up the old black dialer phone and called Dr. DeBakey’s secretary and told her what she had noticed. Next morning at rounds, Dr. DeBakey singled out the resident, held him by the nape of his neck, dragged him to the entrance of the ICU and physically kicked him out of the Unit. The resident was expelled from the program. The reader can make his/her own decision regarding this incident. Was it his strict discipline that he himself practiced and he expected from his students for him to take this drastic action? Was it cruelty? Of course in this day and age this type of authoritarian practice would not be possible without inviting a lawsuit for assault. In fact might be criminal. You decide…..




