By Dr. Kamran Aslam
Tons of great interventional content! Thought I’d add some EP:
Who doesn’t hate vasovagal syncope? Usually, younger patients with little comorbidities, lifestyle changes aren’t always effective, and pacemakers help the HR but the patients still feel poorly. Then young pts have to deal with PPM gen changes, lead issues etc.
Had been doing this in Chicago for a bit, now in Houston: Cardiac Neural Ablation (CNA)
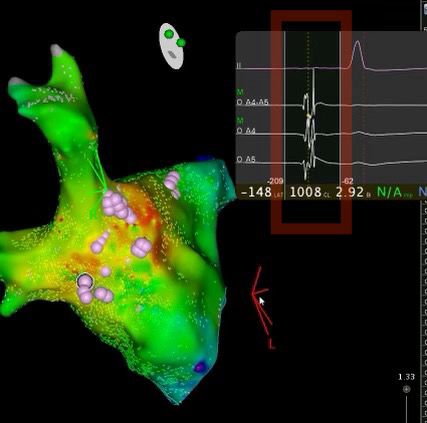
Male pt Mid 30s pt with multiple episodes of VVG syncope, no offending meds, documented drop into junctional with sx. Resting Brady. Referred for pacemaker. One of the screening tools, is giving 1mg atropine to see if there’s a ⬆ HR by at least 10 bpm. He qualified. Took him to EP study. Very detailed electroanatomic map of RA, LA, looking for high fractionated signals in usual anatomical spots posteriorly indicating presence of vagal plexus. Ablation in this area shows response of ⬆ HR during RF 🔥. End point: lack of atropine response. Then clinical observation for sx. Upto 4 patients in Houston now, no recurrence in syncope. None required pacemakers.
My group is part of the international research registry for such pts. Technique recently popularized by Turkish EP in Istanbul: Tolga Aksu
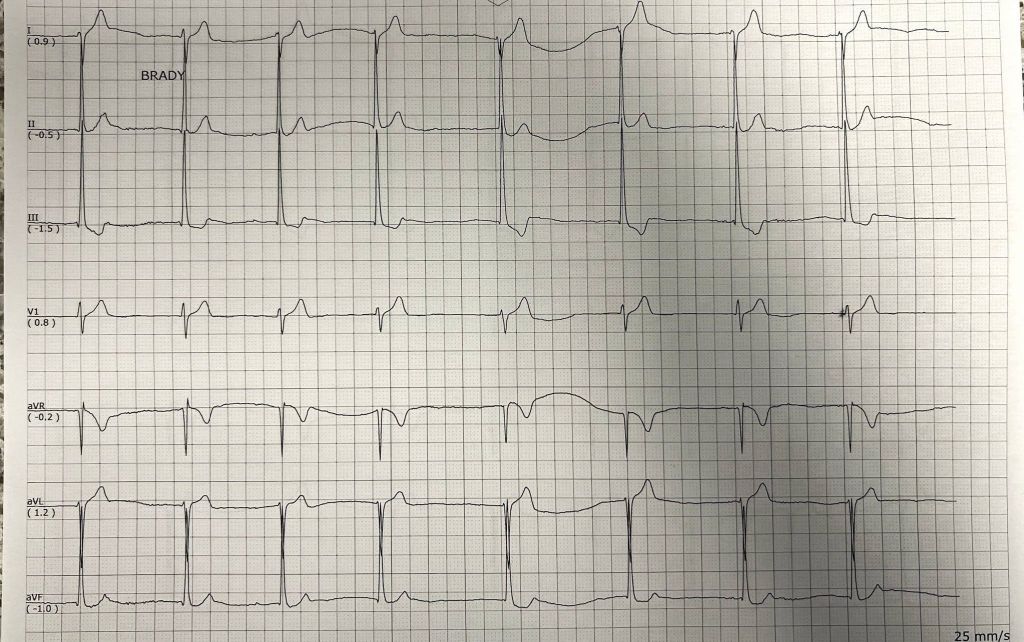
Pics: ECG with sx, Left Atrium with Pink dots = area of burn. The high frequency signals that signature vagal plexii are in the red box, that we hunt for…
once you have vasovagal syncope narrowed down by excluding everything else, removing offending drugs, these are good referrals for further work up
- it’s always nice to have outpatient monitoring correlating sudden bradycardia with symptoms
- a screening tool that I have, baseline, ECG, then IV 1 mg of atropine, With repeat, ECG, you want to see a change of at least 10 to 15 bpm increase in heart rate (these patients benefit most)
- a positive test for a cardio inhibitory syncope is also helpful for the record and to get pre-authorization
- there’s no age range, per se, but these patients tend to be younger, which is a reason for me to try and find a way to make them avoid hardware, specifically a pacemaker
- my last patient interestingly had resting bradycardia and was on fludrocortizone and compression socks, and very interestingly, almost immediately he was able to come off both measures and took his first fishing trip in five years
- A few times, with only a outpatient monitor, showing bradycardia and symptoms, then after mapping, the vagal plexus, with subsequent rapid bursting to stimulate the vagal response was the only way I could prove they could benefit — intra procedure testing… sometimes you just have to prove physiology intra op, just like utility of IVUS, FFR etc…

