By Dr. Salman Arain MD
Here is a way to think (and talk) about left main PCI.
A – Anatomy (i.e. functional anatomy) which includes angiography, IVUS, and physiology.
B – Bifurcation classification If applicable of course.
C – Calcium management. All inclusive term that includes all available devices for lesion preparation: rota, CSI, IVL, cutting balloons, laser, and of course NC balloons.
D – Devices. This includes the need for and choice of mechanical support.
E – Execution. The actual PCI strategy (or strategies).
86 year old man with patent LIMA and SVG to RCA. Now with exertional angina and lateral wall ischemia (large).
Here is the LIMA shot from then – the proximal segment of the LAD is not supplied by the graft. So worth saving and/or protecting.
Here are my ABCDEs – as promised.
A: Functionally and anatomically the calcium involves all three branches. FFR or iFR not needed.
B: This is a Medina 1,1,1. The proximal LAD supplies a significant area and is worth saving.
C: There is nodular calcium and some type of atherectomy will help place stents. My first choice was rotational atherectomy given that it is a front cutter.
D: This is a protected LM and the EF is low normal. So no need for an MCS.
E: The LM is very short or non-existent. This anatomy is better suited for Culotte though any technique would work.
S: Not applicable.
We ended up wiring the LM into the LCX followed by atherectomy with a 1.5 burr. We were unable to wire the proximal LAD from the LM because the ostium was obstructed by the calcium nodule.

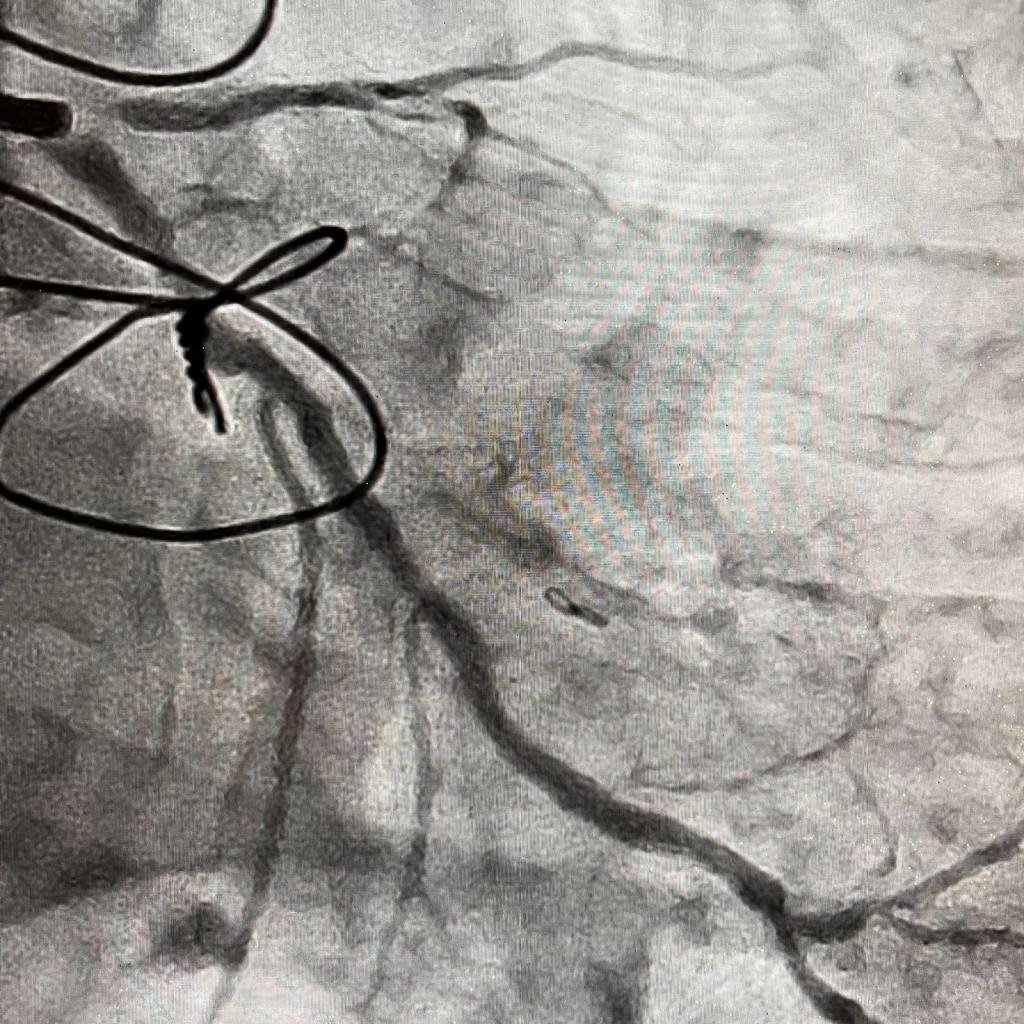
And here is the final result.
You can see that the LCX is technically a first OM that supplies a major portion of the lateral wall with its 5(!) branches.

