By Dr. Salman Arain
Lately we have had several complex (and complicated) RCA interventions. In such cases we usually don’t worry about the RV branch – if it arises from a diseased segment we protect it, if it away we let it be. Also, the transient loss of an RVB is mostly (but not always) well tolerated. Here is a case that is the ‘exception to the rule’.
Introduction: 75 year old man with known CAD. History of RCA PCI (two?) years ago complicated by perforation and placement of a PTFE covered stent. The patient returns with progressive angina.
Interestingly there is severe ISR within the covered stent – which may explain the rather late presentation. Typical ISR presents within 6 to 12 months.
Our plan was to perform PTCA, hopefully provisionally but you can see the difficulty we had advancing even short balloons. We resolved the support issue with a buddy wire and a guide extender.
There was recoil and we decided to stent with an Orsiro (sirolimus based) stent but we had difficulty in advancing it. The RAO reveals why – a ledge of calcium in the mid RCA! We took care of it with lithotripsy (Shockwave).
Shortly after 10 placement, the patient started to complain of chest pain. He also had diffuse ST depression. We repeated the angiogram, but the flow looked good.
We admitted him to the CCU where he had a modest increase in his cardiac enzymes. The high sensitivity troponin went as high as 18,000(!). The levels started to come down on day 2.
The patient continued to complain of exertional jaw pain on day 3. We maximized his antianginals as much as a blood pressure allow, but he continued to be symptomatic. The echo showed normal LV function.
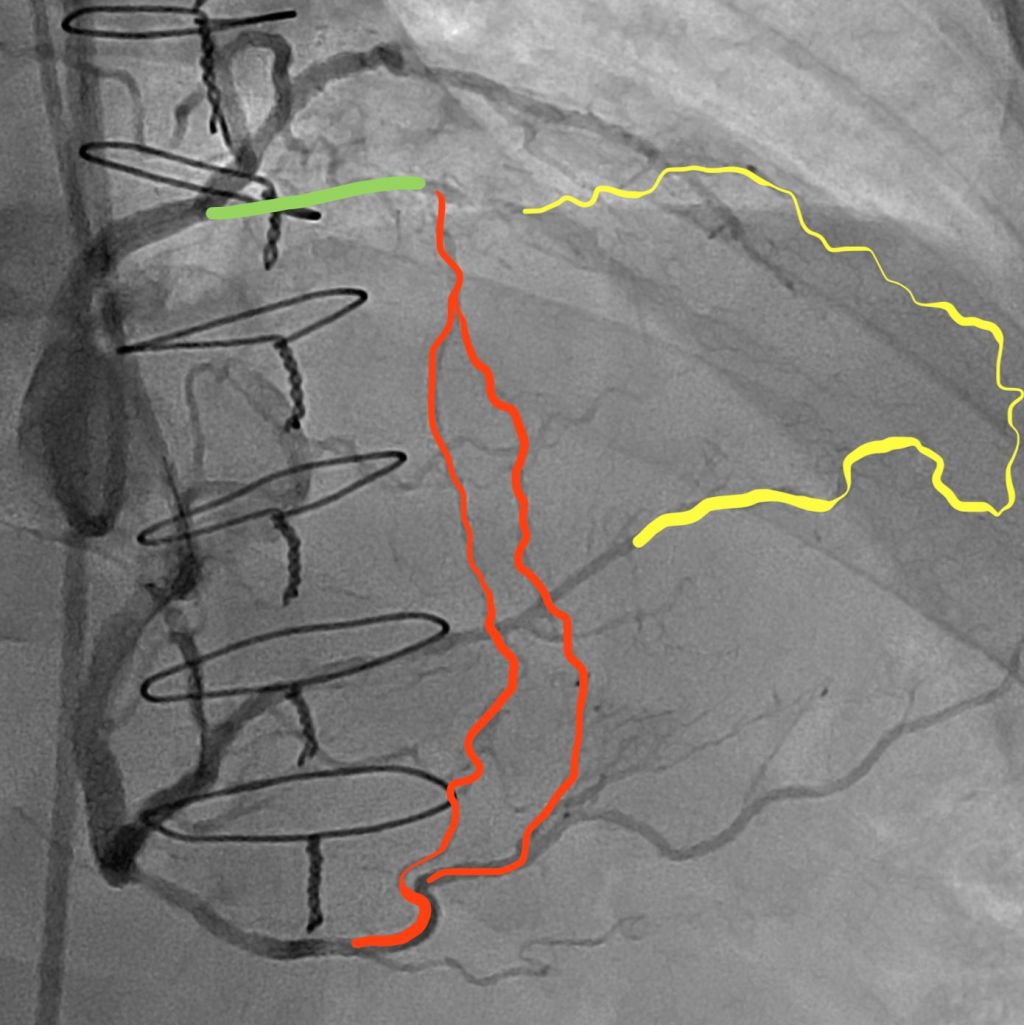
We took the patient back to the lab and found that his RCA was still patent. There is TIMI-2 flow possibly due to the recent PCI and large vessel diameter. However, we can see that there is a small RV branch that had a) disappeared during the first procedure and b) is trying to come back. We decided to open “”rescue it”.
However, this is where things became ‘interesting’. We had considerable difficulty engaging the jailed RVB ostium with multiple wires (both with and without a microcatheter). You can see the challenges here, which include lack of support and a predisposition for wire prolapse.
Some additional thoughts:
1) We took a picture of the left system and it was unchnaged from 3 days ago
2) There were several challenges in wiring: the ostium was jailed, embedded in disrupted calcium, retroflexed or at least perpendicular to the MB, and a relatively wide RCA lumen.
I tried multiple polymer jacketed (slippery) wires to no effect. I even tried a Fighter (0.008 tip) from Boston because it has a non-jacketed tip. For a different grip. But it did not work. With the blocking balloon technique, the wires just kept curling up in the RCA. Also, having a new stent struts did not help – too much exposed metal.
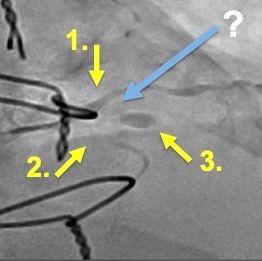
Case Resolution: The Micro JR4!
We decided to try a SuperCross 90 (angle tipped catheter). I gave it a small secondary bend to create a micro JR4, and to our pleasant surprise, it was able to engage the RVB ostium!
Here you can see the micro JR4 in action! We used an anchor balloon to drive the TP LP across the ostium, thus dilating it.
This then allowed us to insert a 1.5 and then a 2 mm ballon. The final angio shows brisk antegrade flow in the recovered RVB.
The patient’s angina resolved completely after the procedure. He felt great and wanted to go home the same day, but we kept him overnight just in case.
An interesting observation: The collateral from the LAD is what kept the distribution of the RVB alive. That is why he continued to have angina, even after the enzymes plateaued. I think it took a day for this collateral to plump up, which is why he suffered immediately after the branch went down.
THE END
What a nice case 👏👏 , masterfully done Salman bhai.
questions
1- would atherectomy have had a lower chance of shutting down side branch compared to lithotripsy
2- did you KISS or POT the RCA after this final ballooning or not needed ?
1) Possibly. Had we used atherectomy, we may have had less disruption at the RV ostium, and we would have cleaved the calcific plaque.
2) I don’t think we did. (Someone else asked and I said yes, but when I checked I couldn’t find the clip).
The goal of the SB balloon was to open the ostium and stretch the struts. Hopefully, the perpendicular takeoff minimized carina shift into the RCA proper.
Great questions Waleed Kayani Bhai. Sometimes we do things “in the heat of the moment” but looking at the case again (alone and with colleagues (like the Houston Cardios!) opens up other possibilities. 😀