From Accidents to Advancements in the Realm of Medications.
Mahmood Syed, MS4
American University School of Medicine
Amanpreet Kaur, MBBS
Government Medical College Patiala, India
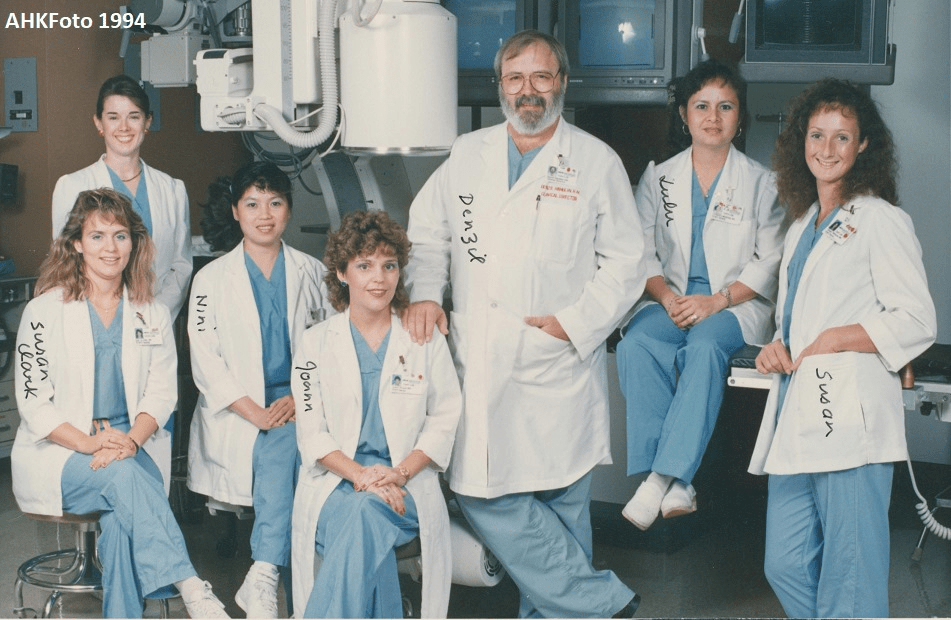
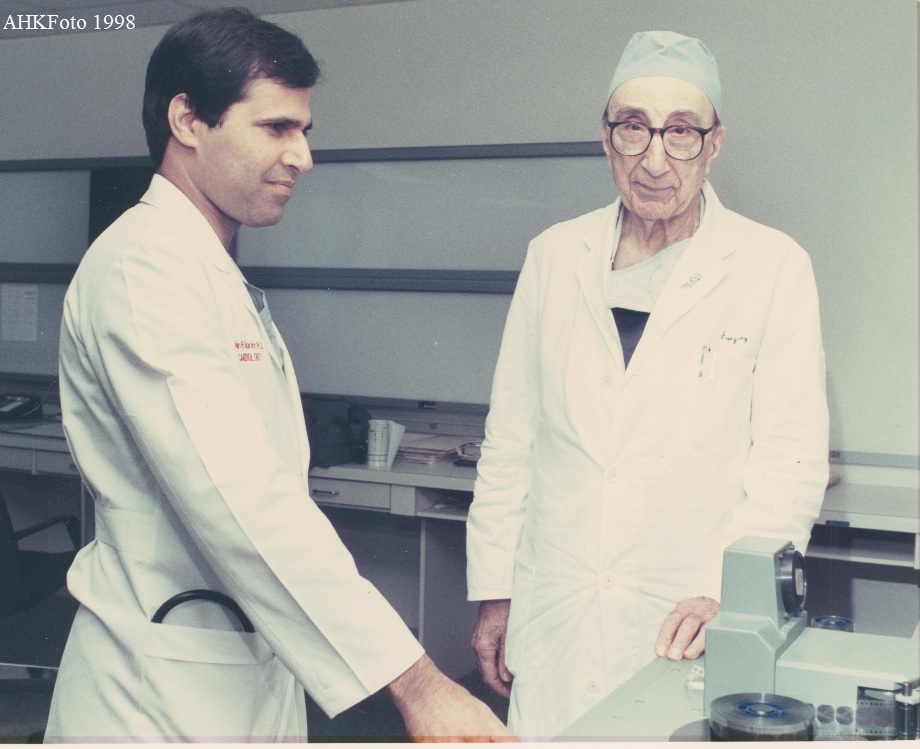
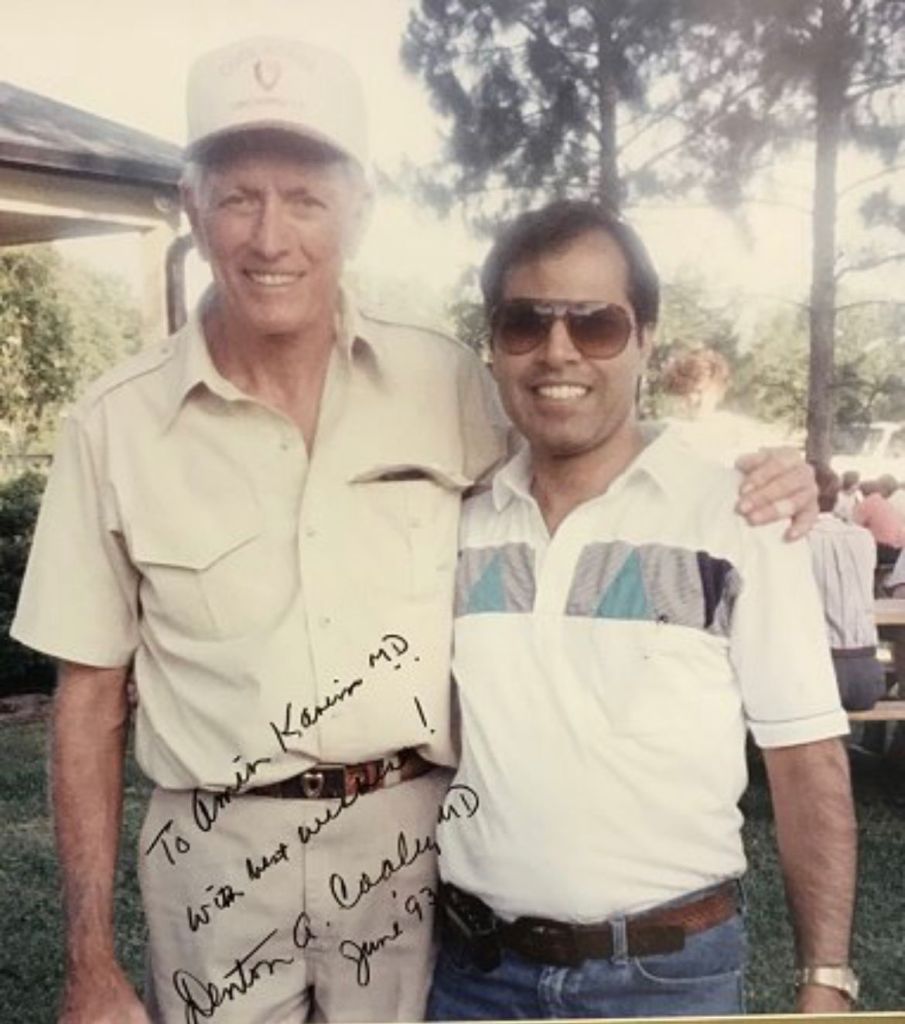
Amin H. Karim MD FACC
Clinical Assistant Professor
Baylor College of Medicine, Houston, Texas.
“When you have acquired knowledge and experience, it is very pleasant to
break the rules and to be able to find something nobody has thought of.”
These were the words of renowned Bacteriologist, Andrew Fleming, who
discovered Penicillin widely used today.
There are drugs whose original discovery was intended for
specific indications. However, their side effects were so
useful that these medications were eventually repurposed as
treatments for other medical conditions. This phenomenon is
also known as “drug repurposing” or “serendipitous
discovery”. Here are some examples of such medications
widely used today:
The discovery of Minoxidil is a fascinating chapter in medicinal
advancements. It was initially created for the treatment of
Hypertension. However, during clinical studies, scientists discovered a
surprising adverse effect that caused hair growth in patients that were
taking this medication. This coincidental finding prompted more
research into Minoxidil’s potential as a male pattern baldness remedy.
Eventually, it was repurposed for this indication.
Viagra (Sildenafil) is another interesting medication that was
unintentionally found while being used in the treatment of Angina
Pectoris and Pulmonary Hypertension. An unanticipated side effect that
the researchers discovered during clinical trials was that many of the
male participants reported having better erectile function after taking this medication due to its vasodilatory effects. Therefore, it was
repurposed as a medication for men suffering from Erectile Dysfunction
(ED).
Bimatoprost was another medication that was initially discovered for the
treatment of Glaucoma, but researchers noted that it increased eyelash
length, thickness, and blackness in the patients who received these eye
drops for the treatment of Glaucoma. This led to its use for cosmetic
enhancement of eyelashes today.
Ozempic (Semaglutide) was originally discovered for the treatment of
Type 2 Diabetes Mellitus. This medication functioned as a GLP-1 agonist.
Researchers found that it caused significant weight reduction in addition
to controlling blood glucose levels. After further clinical trials, it was
approved as a medication for weight loss.
Gabapentin was initially discovered as a potential treatment for seizures
as it was structurally similar to the neurotransmitter GABA. After its
initial discovery, Gabapentin was subsequently found to have efficacy in
treating neuropathic pain in patients who were treated for seizures,
leading to its approval for this indication as well.
Finasteride was initially investigated for its potential use in the
treatment of Benign Prostatic Hyperplasia. While clinical trials were
ongoing to see the effectiveness of this medication for BPH, it was
observed that patients taking finasteride experienced hair growth as a
side effect. Eventually, it was repurposed for the treatment of hair loss.
Methotrexate, a potent inhibitor of Folate metabolism, was used for the
treatment of many cancers including Acute Lymphocytic Leukemia (ALL)
and Choriocarcinoma. It was discovered to be effective in treating
autoimmune conditions due to its ability to inhibit cell growth and
modulate immune responses. Today, it is used to treat conditions like
Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA).
The development of aspirin from a painkiller to a multi-indicated drug is
evidence regarding its healing characteristics. Initially, aspirin was found
to be useful for reducing fever and pain. However, it is now essential for
maintaining cardiovascular health, controlling inflammation, and even
preventing and reducing the incidence of cancer, particularly in the
setting of colon cancer. This extensive range of applications highlights
the significance of aspirin in modern medicine and
its ongoing importance over a century after it was
initially discovered.
There are other medications that produce treatment indications as a result of
their side effect. In the world of ever-evolving medicine and advancements in
medical research, there is no doubt there will be more discoveries of newer
medications as well as current medications with newer indications. The
medical field is expanding on a level never experienced before in humanity. As
new therapies become available, as well as more research being generated as
a result of clinical trials and controlled studies, we will see an even greater
advancement in medicine in the near future than we have ever seen before.
The only limitation that we have is the limitations we set on ourselves. In the
book, The Laws of Medicine, by Pulitzer Prize-winning author Siddhartha
Mukherjee, he says “ In medicine, mistakes are inevitable but learning from
them is essential.” Furthermore, if these mistakes lead to newer discoveries
and treatments in the realm of medicine, then mistakes might just be better
than getting it right the first time.