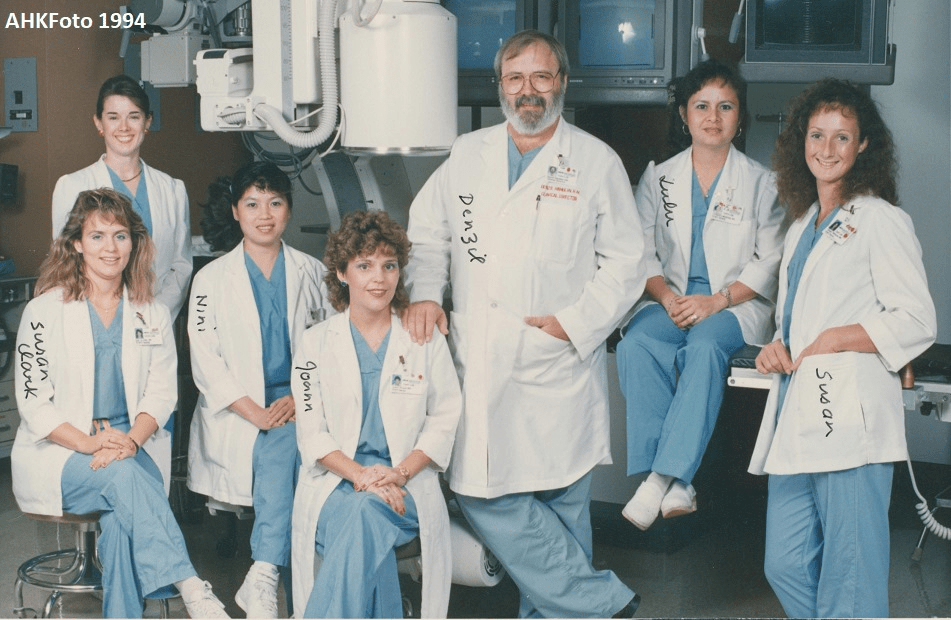
By Amin H. Karim MD
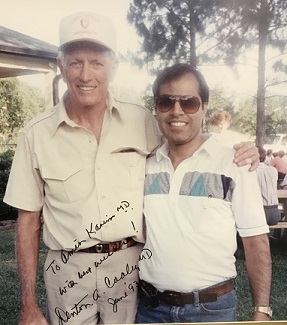
Prof. Michel Mirowski, Chief of Cardiology at the Sinai Hospital of Baltimore, Maryland, Inventor of ICD, with Amin H. Karim (Resident in Department of Internal Medicine 1981)
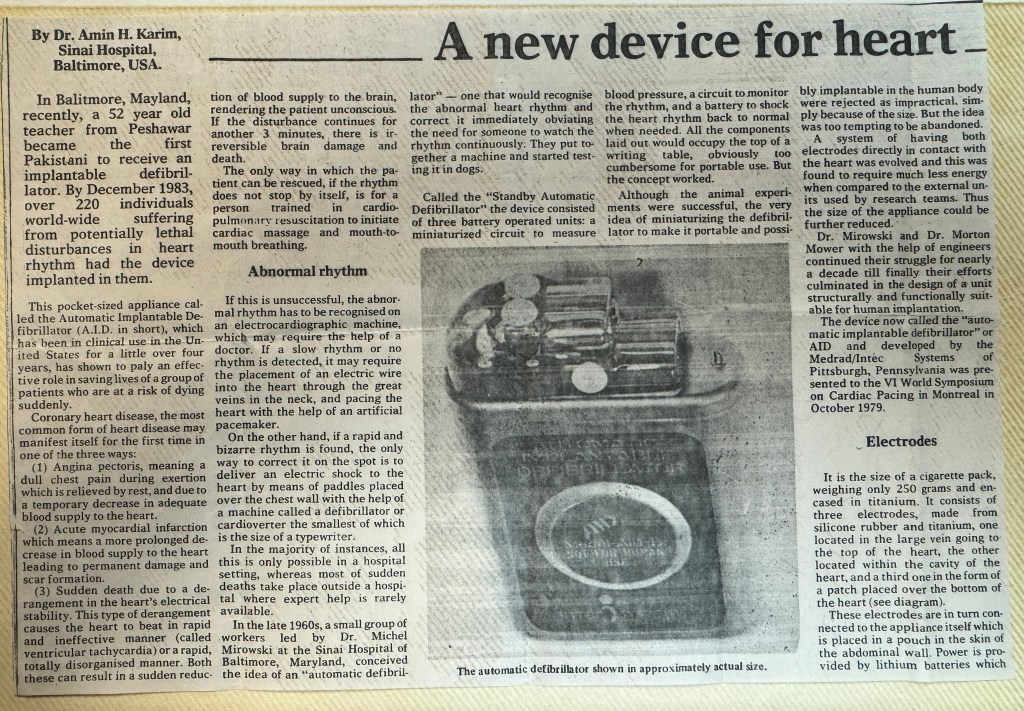
The development of the ICD was pioneered at Sinai Hospital in Baltimore by a team including Michel Mirowski, Morton Mower, Alois Langer, William Staewen, and Joseph “Jack” Lattuca. Mirowski teamed up with Mower and Staewen and together they commenced their research in 1969 but it was 11 years before they treated their first patient.
I was a resident at the Sinai-Hopkins program in 1981-83. We followed the development of the ICD with interest and watched Dr. Mirowski conduct his experiments on dogs. The dog would be attached to electrodes, with a large contraption on a crash cart following the dog. The dog would be put into ventricular tachycardia by stimulation and would collapse to be followed by a auto shock and the dog would be revived! The size of the contraption was the size of a large television; Engineers with Boston Scientic and other companies then worked on it and made it compact and implantable.
The work was commenced against much skepticism even by leading experts in the field of arrhythmias and sudden death. There was doubt that their ideas would ever become a clinical reality. In 1972 Bernard Lown, the inventor of the external defibrillator, and Paul Axelrod stated in the journal Circulation – “The very rare patient who has frequent bouts of ventricular fibrillation is best treated in a coronary care unit and is better served by an effective anti-arrhythmic program or surgical correction of inadequate coronary blood flow or ventricular malfunction. In fact, the implanted defibrillator system represents an imperfect solution in search of a plausible and practical application.”
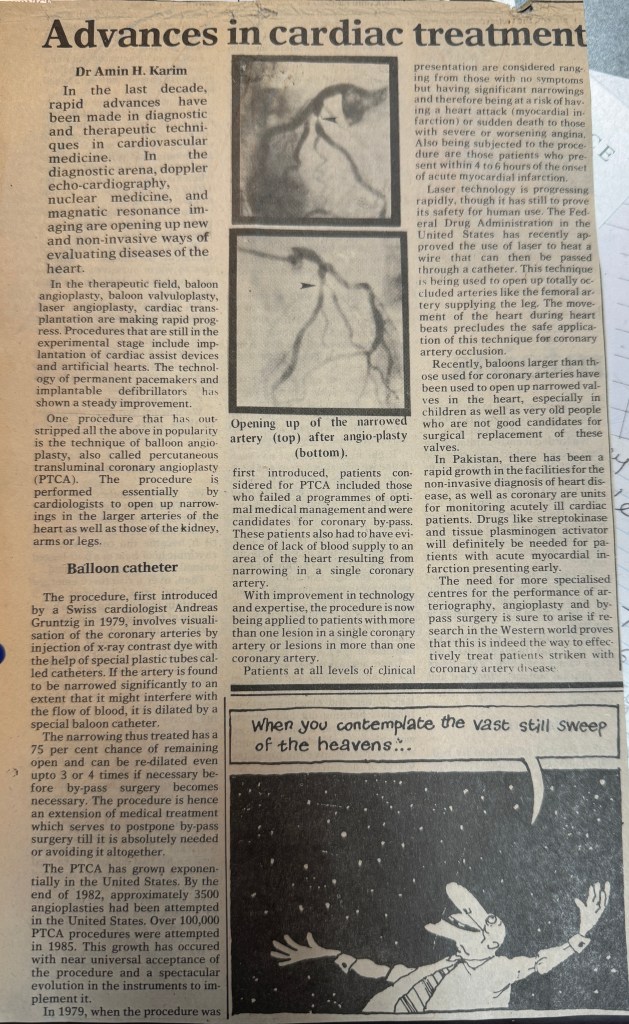
The problems to be overcome were the design of a system which would allow detection of ventricular fibrillation or ventricular tachycardia. Despite the lack of financial backing and grants, they persisted and the first device was implanted in February 1980 at Johns Hopkins Hospital by Dr. Levi Watkins Jr.
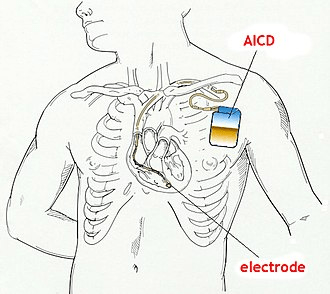
The first devices required the chest to be cut open and a mesh electrode sewn onto the heart; the pulse generator was placed in the abdomen.
ICDs constantly monitor the rate and rhythm of the heart and can deliver therapies, by way of an electrical shock, when the heart rate exceeds a preset number. More modern devices have software designed to attempt a discrimination between ventricular fibrillation and ventricular tachycardia (VT), and may try to pace the heart faster than its intrinsic rate in the case of VT, to try to break the tachycardia before it progresses to ventricular fibrillation. This is known as overdrive pacing, or anti-tachycardia pacing (ATP). ATP is only effective if the underlying rhythm is ventricular tachycardia, and is never effective if the rhythm is ventricular fibrillation.
Many modern ICDs use a combination of various methods to determine if a fast rhythm is normal, supraventricular tachycardia, ventricular tachycardia, or ventricular fibrillation.
Rate discrimination evaluates the rate of the lower chambers of the heart (the ventricles) and compares it to the rate in the upper chambers of the heart (the atria). If the rate in the atria is faster than or equal to the rate in the ventricles, then the rhythm is most likely not ventricular in origin, and is usually more benign. If this is the case, the ICD does not provide any therapy, or withholds it for a programmable length of time.
Rhythm discrimination will see how regular a ventricular tachycardia is. Generally, ventricular tachycardia is regular. If the rhythm is irregular, it is usually due to conduction of an irregular rhythm that originates in the atria, such as atrial fibrillation. In the picture, an example of torsades de pointes can be seen; this represents a form of irregular ventricular tachycardia. In this case, the ICD will rely on rate, not regularity, to make the correct diagnosis.
Morphology discrimination checks the morphology of every ventricular beat and compares it to what the ICD knows is the morphology of normally conducted ventricular impulse for the patient. This normal ventricular impulse is often an average of a multiple of normal beats of the patient acquired in the recent past and known as a template.
The integration of these various parameters is very complex, and clinically, the occurrence of inappropriate therapy is still occasionally seen and a challenge for future software advancements.
Lead II electrocardiogram (known as “rhythm strip”) showing torsades de pointes being shocked by an implantable cardioverter-defibrillator back to the patient’s baseline cardiac rhythm.
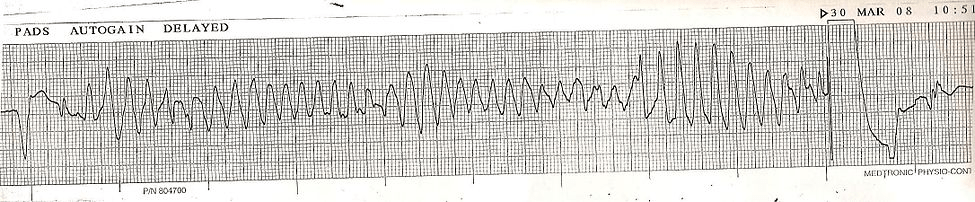
Torsades de Pointes converted by ICD
A number of clinical trials have demonstrated the superiority of the ICD over AAD (antiarrhythmic drugs) in the prevention of death from malignant arrhythmias. The SCD-HeFT trial (published in 2005)showed a significant all-cause mortality benefit for patients with ICD. Congestive heart failure patients that were implanted with an ICD had an all-cause death risk 23% lower than placebo and an absolute decrease in mortality of 7.2 percentage points after five years in the overall population.1 Reporting in 1999, the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial consisted of 1,016 patients, and deaths in those treated with AAD were more frequent (n = 122) compared with deaths in the ICD groups (n = 80, p < 0.001) In 2002 the MADITII trial showed benefit of ICD treatment in patients after myocardial infarction with reduced left ventricular function (EF<30). (Copied from Wikipedia)
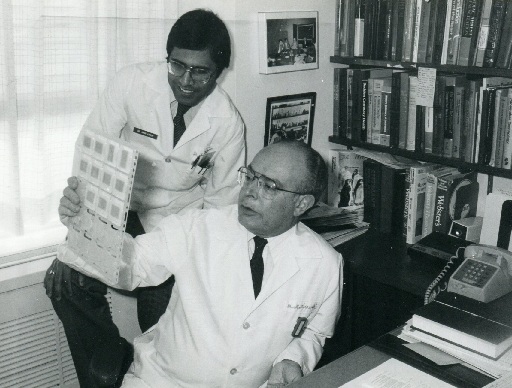
Prof. Mirowski of Sinai Hospital of Baltimore, Maryland in his office.
Mirowski, M; Reid, PR; Mower, MM; Watkins, L; Gott, VL; Schauble, JF; Langer, A; Heilman, MS; Kolenik, SA; Fischell, RE; Weisfeldt, ML (7 August 1980). “Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings”. The New England Journal of Medicine. 303 (6): 322–4. doi:10.1056/nejm198008073030607. PMID 6991948.