RISKS OF VERY LOW LDL CHOLESEROL LEVEL
By Laura Edith Chavez Salas
Universidad De Durango, Campus Zacatecas, Mexico

Amin H. Karim, MD
Houston Methodist Academic Institute
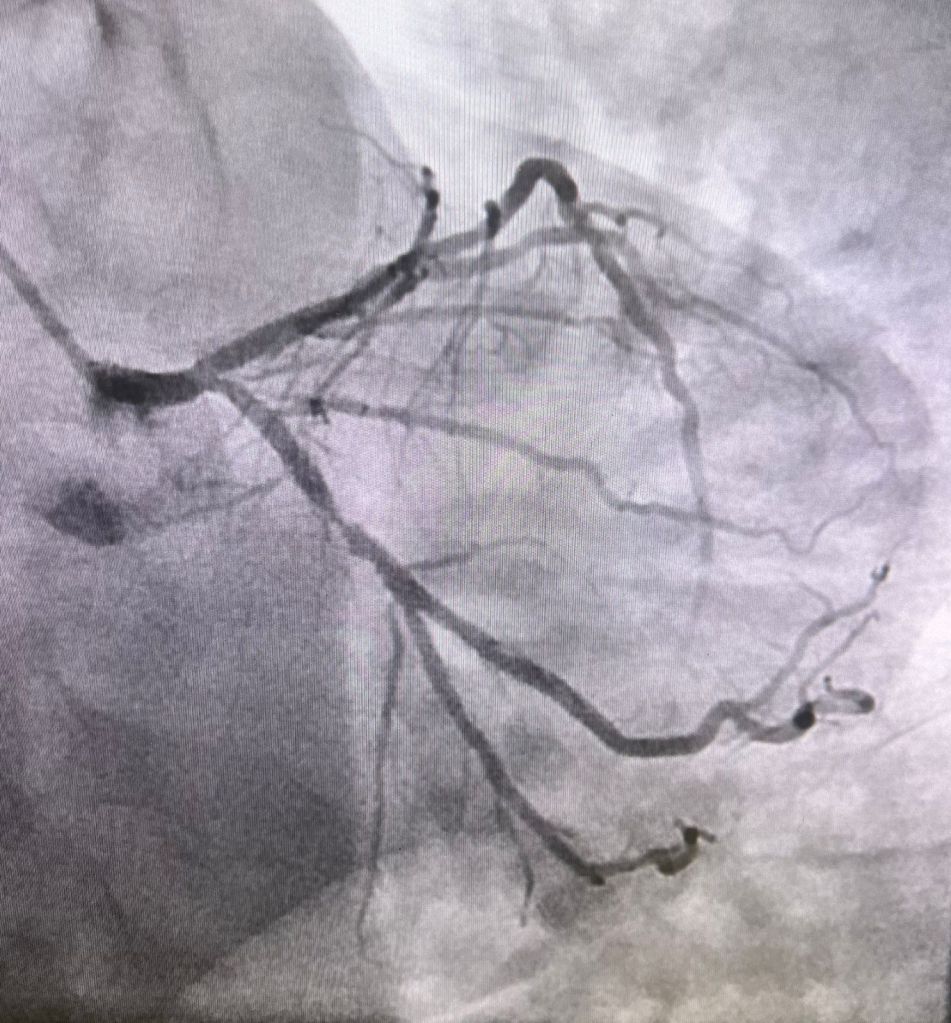
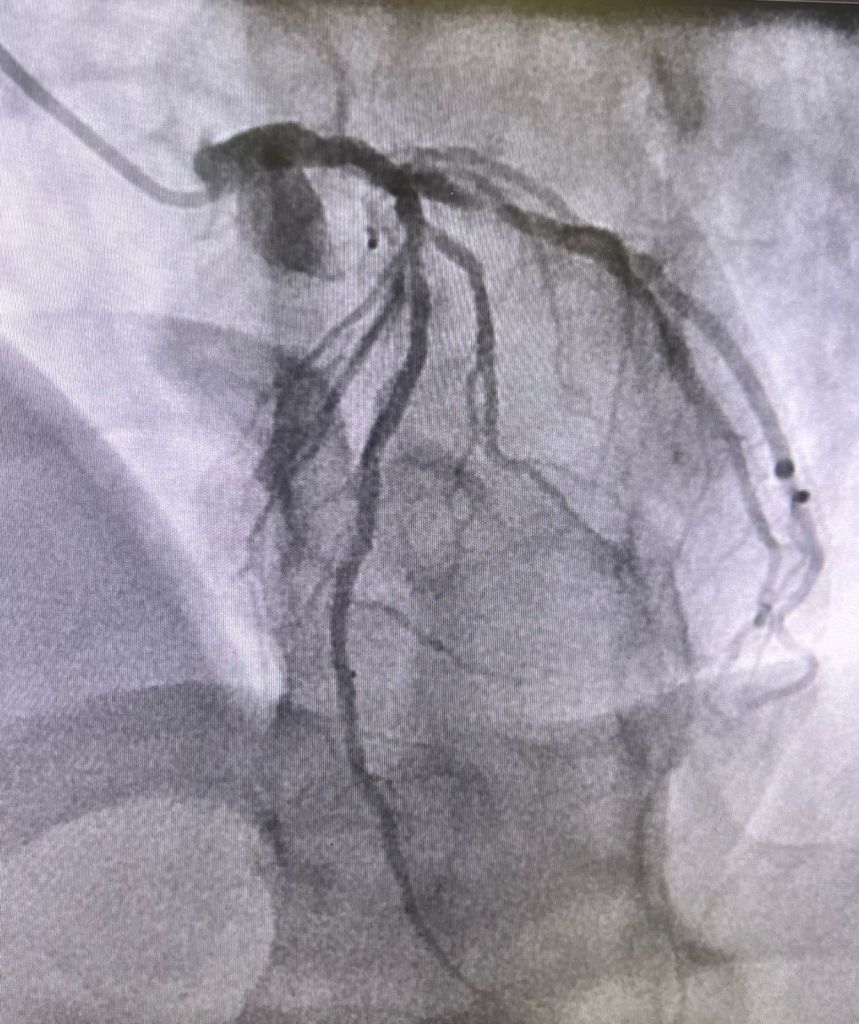
Low-density lipoprotein (LDL) represents a category of lipoprotein particles responsible for the transport of cholesterol and various lipids within the bloodstream. Often referred to as the “bad” cholesterol, it serves vital purposes. LDL particles serve as the primary carriers of cholesterol to peripheral tissues and consist of cholesteryl esters and triglycerides encased in a phospholipid shell, free cholesterol, and a single molecule of apolipoprotein B-100. Increased levels of LDL are directly associated with the onset of atherosclerotic cardiovascular disease (ASCVD), as LDL particles can penetrate the arterial wall, become retained and altered (for instance, oxidized), and facilitate the development of foam cells and atherosclerotic plaques. (1-4)
LDL exhibits heterogeneity, with subclasses that vary in size and density; smaller, denser LDL particles are deemed more atherogenic compared to their larger, more buoyant counterparts. (3, 5, 6) The cholesterol content within LDL particles is quantified as LDL cholesterol (LDL-C), which serves as a conventional marker for evaluating and managing cardiovascular risk. (7) Nevertheless, the quantity of LDL particles (LDL-P) and the concentration of apolipoprotein B (apoB) may offer further risk stratification, particularly in individuals with metabolic syndrome or diabetes, as discrepancies between LDL-C and LDL-P can arise. (8) Evaluation of ASCVD risk can be evaluated by assessing both LDL-C and LDL-P, asserting that the reduction of LDL—primarily through the use of statins and other lipid-lowering treatments—leads to a decrease in cardiovascular events. (4)
DANGERS OF VERY LOW LDL
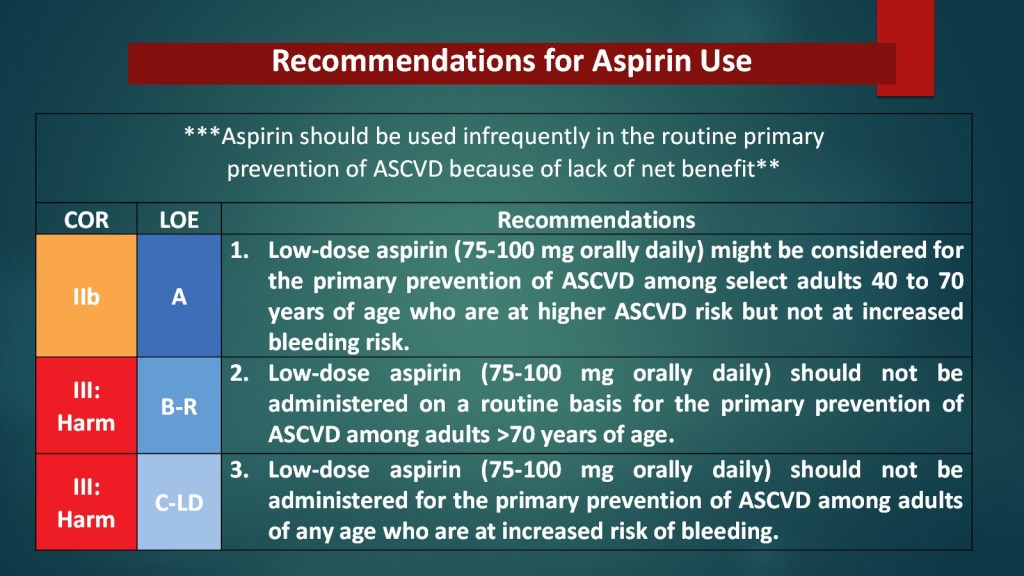
However, an LDL-lowering regimen can lead to ultra-low-density lipoprotein cholesterol (LDL-C) levels. These are typically defined as <40–50 mg/dL, and especially <30 mg/dL. These levels are generally well tolerated and associated with a reduced risk of atherosclerotic cardiovascular disease (ASCVD), but several potential dangers have been identified. (9) Mechanistically, very low LDL-C may impair endothelial integrity and platelet function. This could potentially increase bleeding risk, especially for intracranial and gastrointestinal hemorrhage. (10, 11)
The most observed danger of ultra-low LDL is a possible hemorrhagic stroke and other bleeding events, particularly at LDL-C levels below 40 mg/dL, as supported by mechanistic and clinical data. Observational studies and meta-analyses have also reported a U-shaped relationship between LDL-C and all-cause mortality, with both very low (<50 mg/dL) and high (≥130 mg/dL) LDL-C levels associated with increased mortality in certain populations, such as those with coronary artery disease. (15)
There is also some evidence suggesting a potential association between ultra-low LDL-C and increased risk of new-onset diabetes mellitus, particularly with statin therapy. Leading to more complications, there is a possible link to cataract formation and glaucoma, though causality remains unproven and the absolute risk is low. (11, 14)
The main dangers of ultra-low LDL-C are a possible increased risk of hemorrhagic stroke, new-onset diabetes, and, less consistently, all-cause mortality in specific populations. However, for most high-risk patients, the cardiovascular benefits of aggressive LDL-C lowering outweigh these potential risks. (9-14)
HIGH-RISK PATIENTS
Patients at highest risk for complications associated with very low levels of low-density lipoprotein cholesterol (LDL-C) are:
• Individuals with a prior history of hemorrhagic stroke:
The American Stroke Association notes that the risk of hemorrhagic stroke with statin therapy is small and nonsignificant in those without prior cerebrovascular disease, but patients with a history of hemorrhagic stroke may be at increased risk, and lipid lowering in this group requires individualized consideration and further study. (16)
• Patients with poorly controlled hypertension and very low LDL-C:
There is literature that indicates that the combination of very low LDL-C (especially ≤40 mg/dL) and uncontrolled hypertension substantially increases the risk of both ischemic and hemorrhagic stroke. Although this risk is particularly more prevalent in East Asian populations, it is relevant globally. (17)
• Women with LDL-C <70 mg/dL:
There is evidence from long-term cohort studies in women that has shown that LDL-C <70 mg/dL is associated with a more than twofold increased risk of hemorrhagic stroke compared to LDL-C 100–129.9 mg/dL, independent of other risk factors. Meaning that women with no other risk factors have more risk than males with no other risk factors. (18)
• Patients on intensive statin therapy or with other risk factors for diabetes: Statin therapy, especially at high intensity, is associated with a modestly increased risk of new-onset diabetes. Particularly in those with predisposing factors such as metabolic syndrome or impaired fasting glucose. (11)
Risks associated with having ultra-low LDL-C are more prevalent in populations most at risk, which are those with prior hemorrhagic stroke, poorly controlled hypertension, women, and individuals with multiple vascular risk factors or on intensive lipid-lowering therapy.
REFERENCES
- Orlova, E V et al. “Three-dimensional structure of low density lipoproteins by electron cryomicroscopy.” Proceedings of the National Academy of Sciences of the United States of America vol. 96,15 (1999): 8420-5. doi:10.1073/pnas.96.15.8420
- Rhainds, D, and L Brissette. “Low density lipoprotein uptake: holoparticle and cholesteryl ester selective uptake.” The international journal of biochemistry & cell biology vol. 31,9 (1999): 915-31. doi:10.1016/s1357-2725(99)00046-1
- Qiao, Ya-Nan et al. “Low-density lipoprotein particles in atherosclerosis.” Frontiers in physiology vol. 13 931931. 30 Aug. 2022, doi:10.3389/fphys.2022.931931
- Maurya, Rupesh et al. “Low density lipoprotein receptor endocytosis in cardiovascular disease and the factors affecting LDL levels.” Progress in molecular biology and translational science vol. 194 (2023): 333-345. doi:10.1016/bs.pmbts.2022.09.010
- Ivanova, Ekaterina A et al. “Small Dense Low-Density Lipoprotein as Biomarker for Atherosclerotic Diseases.” Oxidative medicine and cellular longevity vol. 2017 (2017): 1273042. doi:10.1155/2017/1273042
- Packard, C et al. “The role of small, dense low density lipoprotein (LDL): a new look.” International journal of cardiology vol. 74 Suppl 1 (2000): S17-22. doi:10.1016/s0167-5273(99)00107-2
- Jialal, I, and A T Remaley. “Measurement of low-density lipoprotein cholesterol in assessment and management of cardiovascular disease risk.” Clinical pharmacology and therapeutics vol. 96,1 (2014): 20-2. doi:10.1038/clpt.2014.69
- Galimberti, Federica et al. “Apolipoprotein B compared with low-density lipoprotein cholesterol in the atherosclerotic cardiovascular diseases risk assessment.” Pharmacological research vol. 195 (2023): 106873. doi:10.1016/j.phrs.2023.106873
- Karagiannis, Angelos D et al. “How low is safe? The frontier of very low (<30 mg/dL) LDL cholesterol.” European heart journal vol. 42,22 (2021): 2154-2169. doi:10.1093/eurheartj/ehaa1080
- Siniscalchi, Carmine et al. “Low LDL-Cholesterol and Hemorrhagic Risk: Mechanistic Insights and Clinical Perspectives.” International journal of molecular sciences vol. 26,12 5612. 11 Jun. 2025, doi:10.3390/ijms26125612
- Cure, Erkan, and Medine Cumhur Cure. “Emerging risks of lipid-lowering therapy and low LDL levels: implications for eye, brain, and new-onset diabetes.” Lipids in health and disease vol. 24,1 185. 21 May. 2025, doi:10.1186/s12944-025-02606-6
- Olsson, A G et al. “Can LDL cholesterol be too low? Possible risks of extremely low levels.” Journal of internal medicine vol. 281,6 (2017): 534-553. doi:10.1111/joim.12614
- Rong, Shuang et al. “Association of Low-Density Lipoprotein Cholesterol Levels with More than 20-Year Risk of Cardiovascular and All-Cause Mortality in the General Population.” Journal of the American Heart Association vol. 11,15 (2022): e023690. doi:10.1161/JAHA.121.023690
- Faselis, Charles et al. “Is very low LDL-C harmful?.” Current pharmaceutical design vol. 24,31 (2018): 3658-3664. doi:10.2174/1381612824666181008110643
- Scudeler, Thiago Luis et al. “Association between low-density lipoprotein cholesterol levels and all-cause mortality in patients with coronary artery disease: a real-world analysis using data from an international network.” Scientific reports vol. 14,1 29201. 25 Nov. 2024, doi:10.1038/s41598-024-80578-w
- Goldstein, Larry B., et al. “Aggressive LDL-C Lowering and the Brain: Impact on Risk for Dementia and Hemorrhagic Stroke: A Scientific Statement From the American Heart Association.” Arteriosclerosis Thrombosis and Vascular Biology, vol. 43, no. 10, Sept. 2023, https://doi.org/10.1161/atv.0000000000000164.
- Wu, Zhijun et al. “The risk of ischemic stroke and hemorrhagic stroke in Chinese adults with low-density lipoprotein cholesterol concentrations < 70 mg/dL.” BMC medicine vol. 19,1 142. 16 Jun. 2021, doi:10.1186/s12916-021-02014-4
- Rist, Pamela M et al. “Lipid levels and the risk of hemorrhagic stroke among women.” Neurology vol. 92,19 (2019): e2286-e2294. doi:10.1212/WNL.0000000000007454