Amin H. Karim MD
Institute for Academic Medicine
Houston, Texas
Today a 65 year old patient showed up in the office. He had not seen me for last 5 years for whatever reason and now needed a surgical clearance. He worked as a RN at a Houston Hospital and subsequently at the VA Hospital;
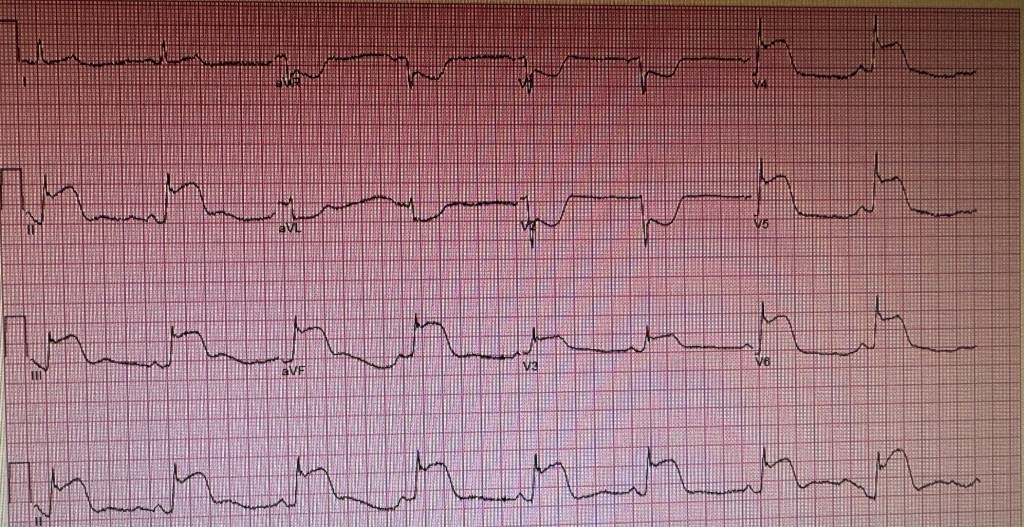
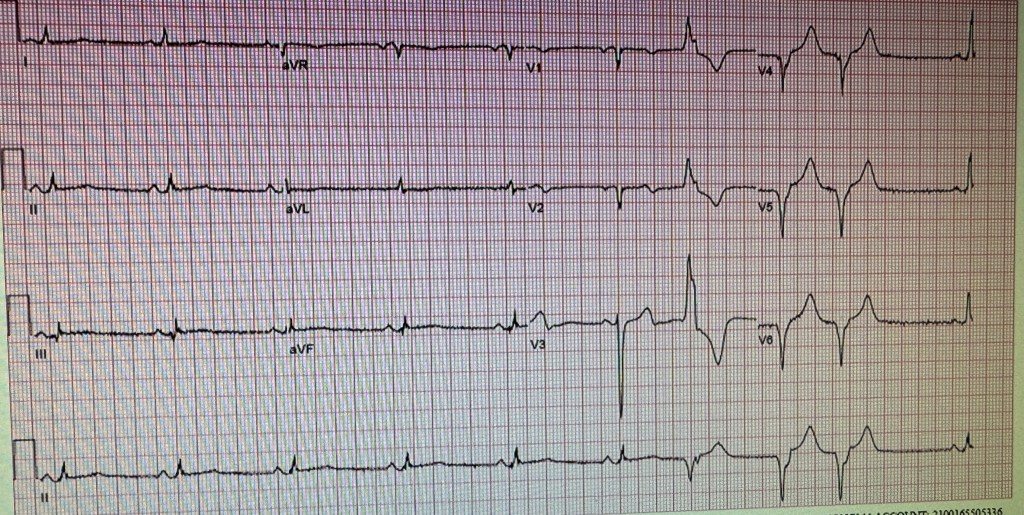
I did a routine EKG as follows:
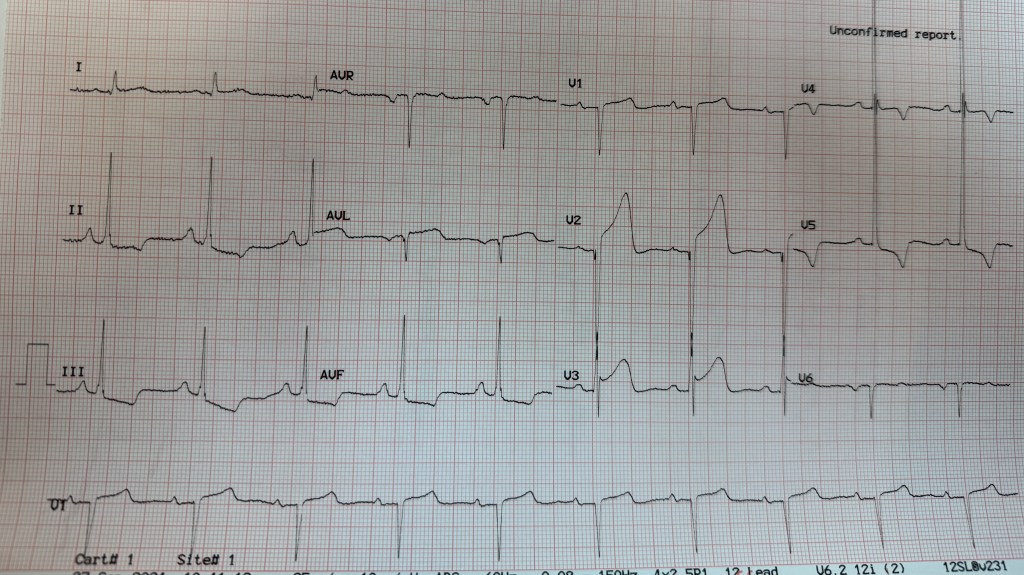
It was unchanged from his previous EKGs from years ago. When he was following with me, he had a cardiac workup including imaging tests showing normal coronaries.
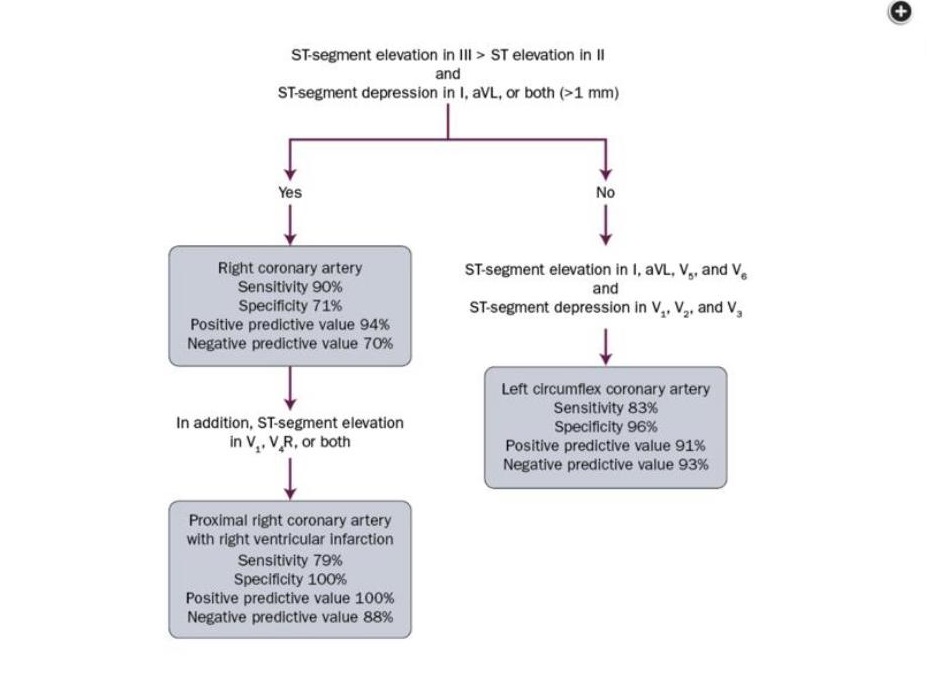
On taking his interval history, I found some interesting facts. While working at the VA he had some atypical chest pain. He went to the ER and had an EKG and was seen by a cardiologist stat. He was rushed to the catheterization lab and had a diagnostic cardiac catheterization which showed normal coronaries. A few months later he had similar chest pain and again went to the ER at a premier hospital in town for evaluation. An EKG was done and STEMI was called immediately. He protested to the cardiologist that he had cardiac catheterization a few months ago and that it was normal! The cardiologist was insistent that he have another one since his EKG showed that he was having a heart attack and could die. His protests were to no avail and he was rushed to the lab and had another diagnostic cardiac study which of course showed normal coronaries. The cardiologist came and apologised to him for not listening to him.
Now it was my turn to beat him on the head and tell him: ” You have STEMI written on your forehead. Wherever, you go you will be treated with emergency response and the STEMI will be summoned and you will be rushed in an elevator with a security guard holding it! Once in the cath lab you will be surrounded by a frantic team counting minutes!
So this is what you are going to do. You will take a copy of your EKG, go to Office Depot and have it reduced and laminated; then carry it with you in your wallet and if you land in the ER and before they wheel you away to the cath lab, show them the EKG and tell them that your EKG is always abnormal and that they should compare to see if there are any changes. Otherwise you will someday end up with a clot in your hand or leg or some other complication!
I think he got the message.
No offence meant and take it in the lighter vein, but I am sure every interventional cardiologist taking emergency calls faces these alarms and the 90 minutes door to balloon time does not allow much margin to hunt for old EKGs!
Amin H. Karim MD
September 27 2024