By Paulina Maldonado
Universidad De Durango, Chihuahua, Mexico
Houston, Texas.
Amin H. Karim MD
Baylor College of Medicine and
Methodist Institute of Academic Medicine, Houston, Texas
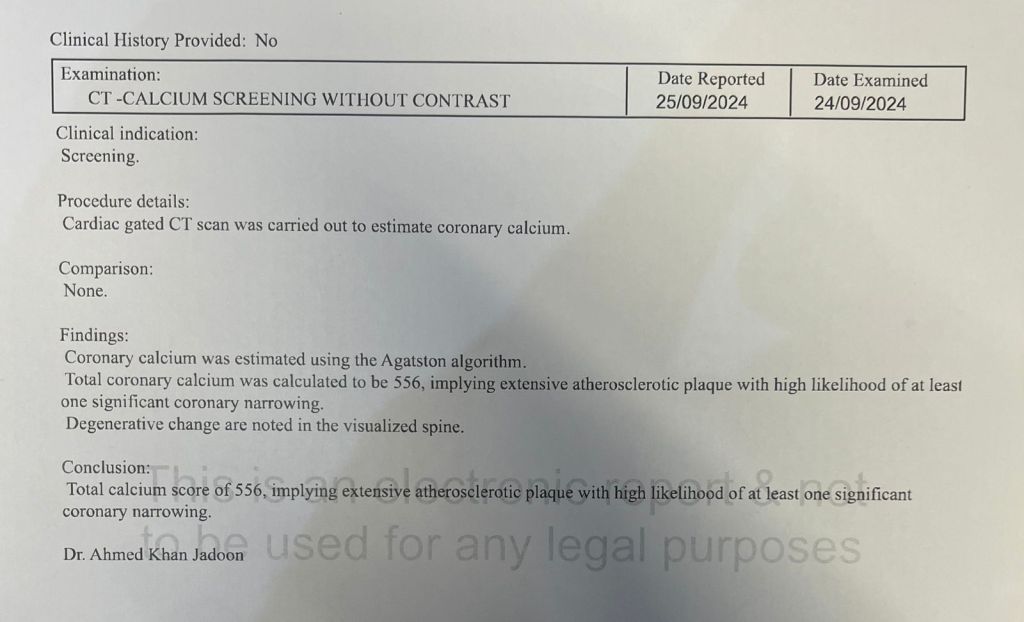
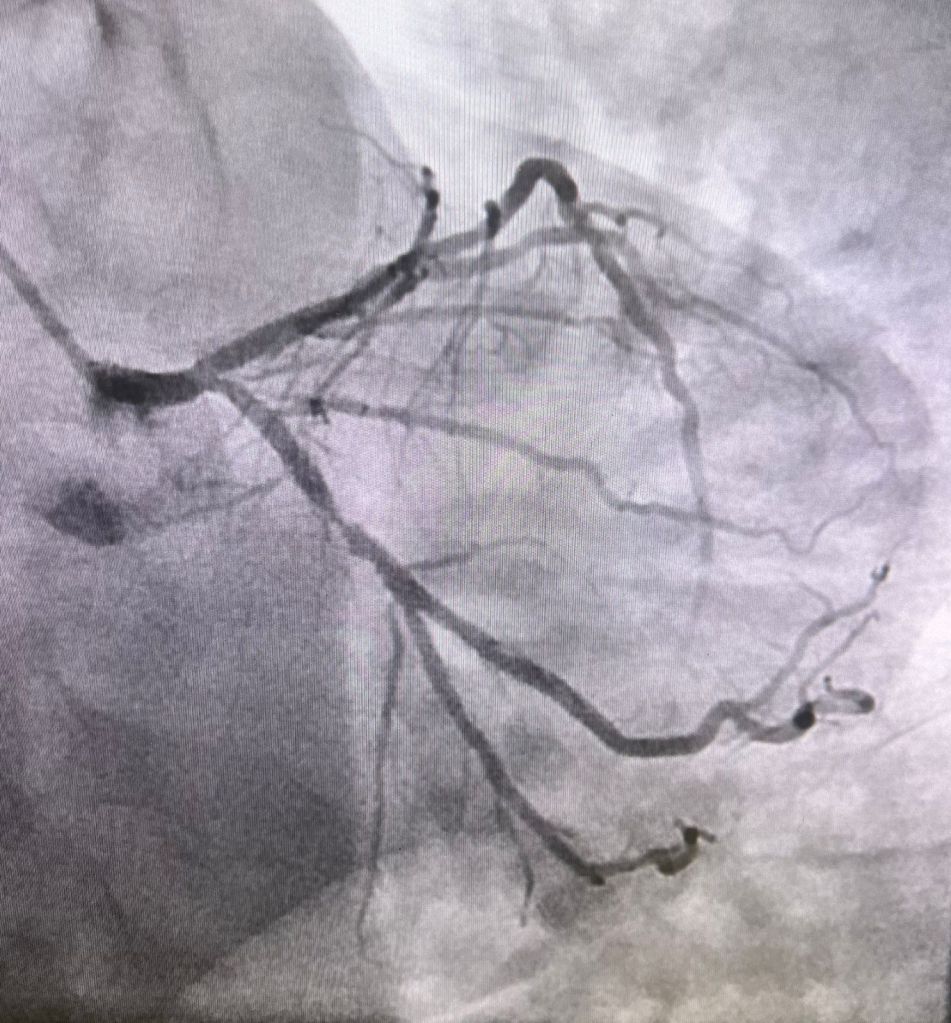
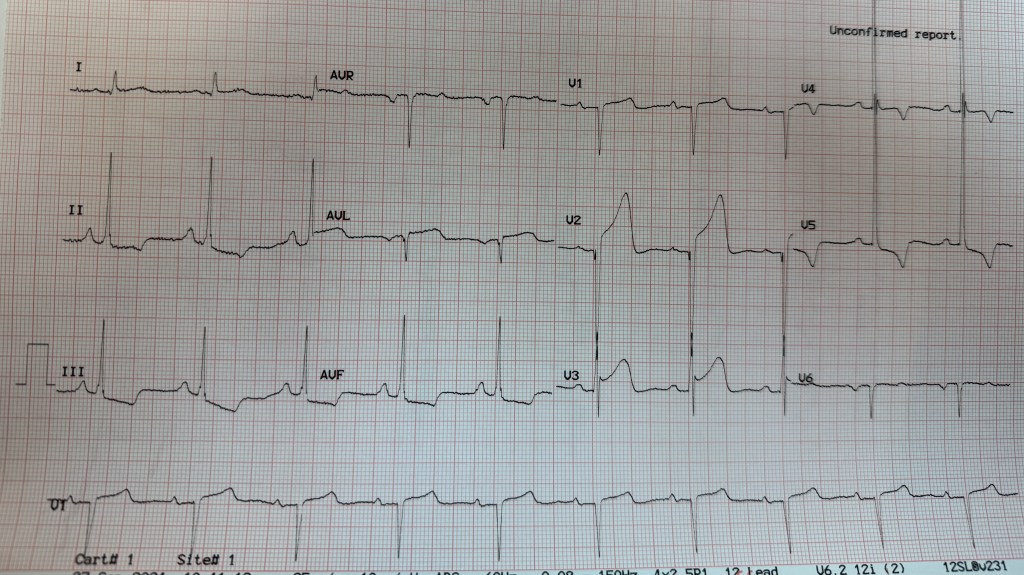
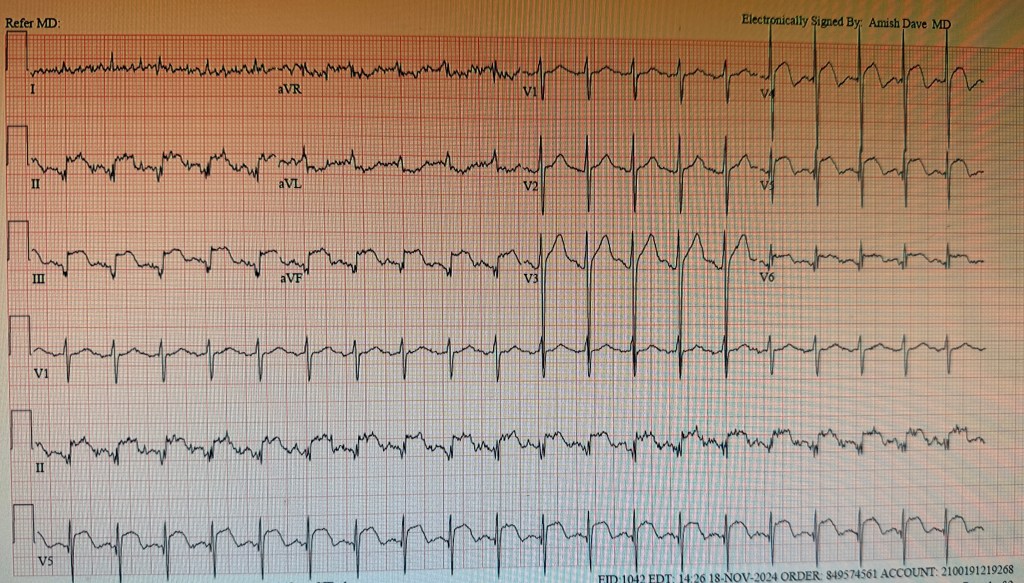
A 65 year old patient presented, disabled from old cerebro vascular accident causing flaccid left sided hemiplegia with contractures, admitted to hospital for change of mental status; he developed hypotension; EKG showed ST elevation in II, III and aVF as well as V3V4V5 diagnostic of inferior wall myocardial infarction with lateral extension.
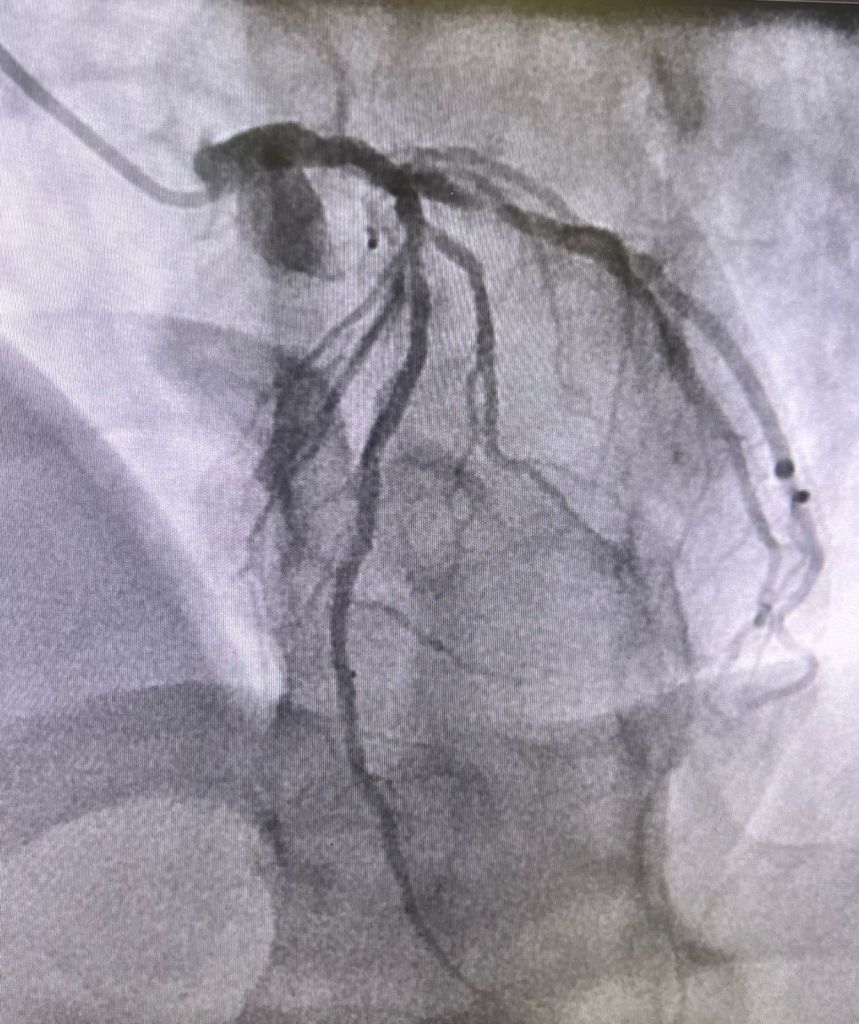
He was rushed to the cath lab where cardiac catheterization showed what looked like “normal coronary arteries”.
His high sensitivity peaked at 1200. He was treated with intravenous heparin and beta blockers; he remained hemodynamically stable and was discharged.
Myocardial Infarction with nonobstructive coronary atherosclerosis
Although the occurrence was initially reported about 80 years ago a very small number of patients are found to have MINOCA.
The term MINOCA is reserved for patients with elevated troponin associated with myocardial ischemia at presentation and should not include disorders with non ischemic elevated troponin.
It is important to mention and reiterate that MINOCA should not be considered a final diagnosis but rather a working one that requires further testing.
Epidemiology
The incidence of MINOCA varied from 1% to 15% and roughly 6% of all Acute Myocardial Infarction cases.
- Younger (18-55)
- Female
- lower prevalence of hyperlipidemia
- ⅓ presented with ST segment elevation of myocardial infarction
Pathogenesis:
MINOCA is heterogenous and can be divided into coronary, cardiac and extra cardiac causes. Ischemia happens during a temporary suspension of blood flow to the myocardium and it takes place in the epicardial arteries or the microvasculature.
| Coronary | Cardiac | Extra cardiac |
|---|---|---|
| plaque rupture or erosion | Myocarditis | stroke |
| coronary spasm | Takotsubo syndrome | pulmonary embolism |
| spontaneous coronary artery dissection | cardiomyopathies | sepsis |
| coronary embolization | cardiac trauma | renal failure |
| coronary microvascular disorders | tachyarrhythmias | hypoxemia |
Risk factors:
- Associated with Long term major adverse cardiovascular events after MINOCA including ST segment elevation on a presenting Electrocardiogram
- older age
- reduced left ventricular ejection fraction
- diabetes mellitus
- hypertension
- tobacco use
- prior Myocardial infarction
- Stroke
- peripheral artery disease
- chronic obstructive pulmonary disease
- chronic kidney disease
- lower total cholesterol
- Peak troponin
- Depression at the time of MINOCA
Signs and Symptoms:
- Chest pain/chest pressure / chest heaviness
- Nausea
- jaw, neck or upper back pain
- pain or pressure in the lower chest or upper abdomen
- shortness of breath
- fainting
- indigestion
- fatigue
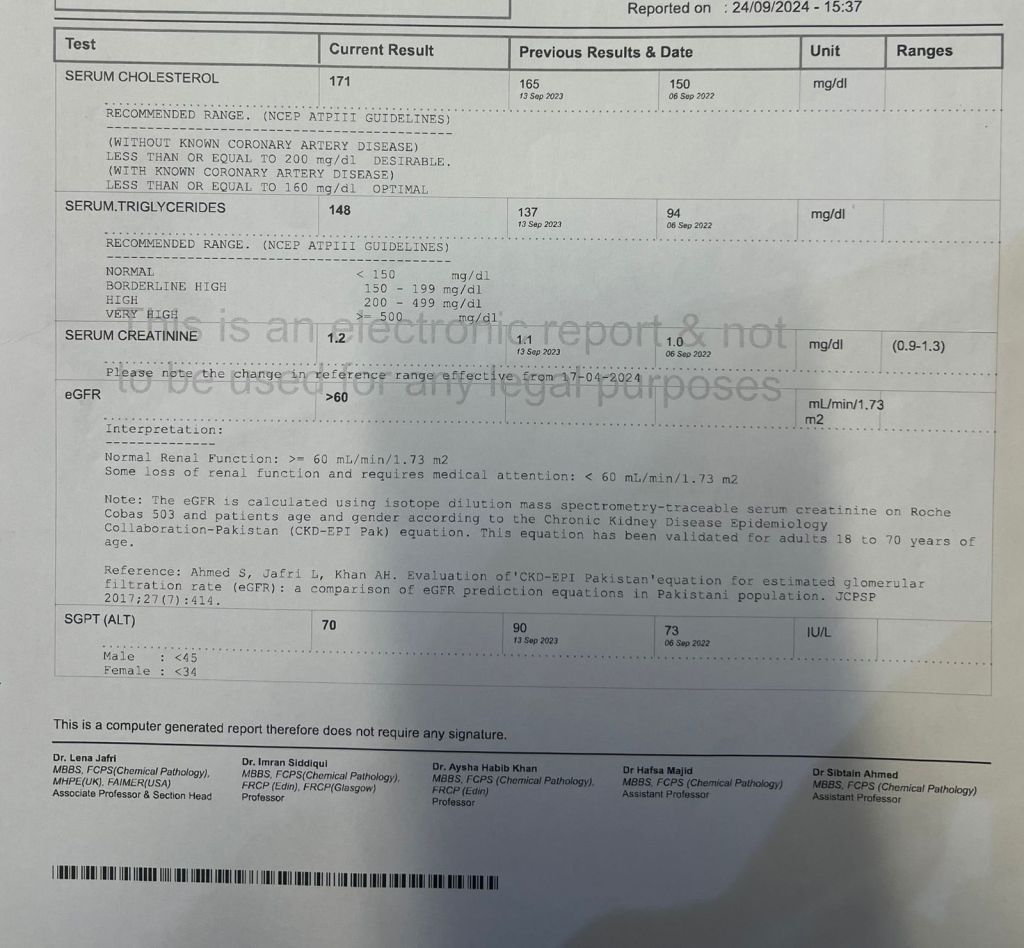
Diagnostics:
Requires a comprehensive diagnostic workup. Is the first line diagnostic tool to detect non obstructive epicardial coronary arteries (less than 50% stenosis) in the setting of an Myocardial Infarction.
Imagining modalities are vital in diagnosing and identifying the underlying mechanisms of MINOCA.
Coronary intravascular imaging
With Intravascular Ultrasound 40% cases and Optical Coherence Tomography 50% cases is essential to diagnose plaque disruption.
It should be performed at the time of coronary angiography for Acute Myocardial Infarction in all 3 major epicardial arteries.
Cardiac Imaging
Transthoracic echocardiography used in the assessment of cardiac function after a MINOCA. It can be used in the diagnosis of Takotsubo cardiomyopathy and non ischemic cardiomyopathy specifically to demonstrate recovery of left ventricular function.
Transesophageal echocardiography can be used when coronary embolism is suspected.
Cardiac Magnetic Resonance Imagining (CMRI) provides a diagnosis in 74-87% of all MINOCA patients.
- Subendocardial (or transmural) pattern of myocardial edema, inflammation or fibrosis is suggested of ischemic Myocardial Infarction.
- Epicardial pattern is suggestive of non ischemic Myocardial Infarction.
Echocardiogram can be used to diagnose Takotsubo cardiomyopathy and non ischemic cardiomyopathy, but CMRI can only be used to detect myocarditis.
Myocardial perfusion quantification with adenosine or regadenoson can be used to diagnose coronary microvascular dysfunction non invasively.
The timing to perform a CMRI is important; it should be completed as close to the acute myocardial infarction as possible. CMRI carries not only diagnostic value but prognostic value as well.
Multimodality approach
OCT and CMRI together resulted in a diagnosis in 85% of the cases whereas Optical Coherence Tomography alone was only 46% and Cardiac Magnetic Resonance Imagining 74%.
Treatment
It should me customized to the underlying diagnosis:
| Meds | Underlying diagnosis |
|---|---|
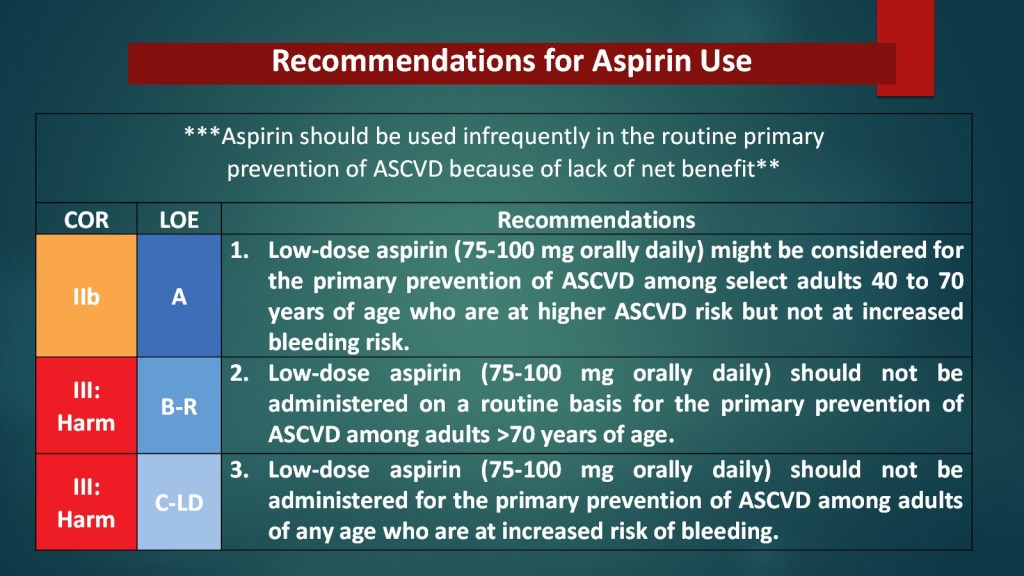
| Aspirin and High intensity statins | Plaque disruption |
| dual antiplatelet therapy by adding ticagrelor for less than 1 month | Plaque disruption not undergoing stenting |
| Beta blocker and renin angiotensin system inhibitors | left ventricular dysfunction |
| Long acting calcium channel antagonist (dihydropyridine and nondihydropyridine) | MINOCA patients secondary to epicardial coronary vasospasm |
| nitrates can be added to calcium channel antagonists | refractory variant angina |
| antithrombotic agents | coronary embolism or thrombosis |
| targeted therapies | underlying thrombophilia |
| conservative management (avoiding increased risk of complications with intervention) | spontaneous coronary artery dissection |
| Percutaneous coronary intervention | STEMI, cardiogenic shock, ongoing ischemia |
| aspirin, beta blocker, statin and renin angiotensin system | spontaneous coronary artery dissection (should be assessed based on individual risk factors |
| antianginal treatment with b blockers, calcium, channel antagonists and ranolazine | Chest pain |
| MINOCA mimickers | Heart failure |
| mechanical circulatory support | progressive circulatory failure |
| resolves in most patients within 2-4 weeks | Myocarditis, but if they develop arrhythmia and persistent cardiac dysfunction medical therapy should be administered. |
| antivirals and immunosuppressives | underlying etiologies |
Prognosis:
Short and long term mortality
At 1 year follow up, MINOCA mortality is 2 to 5%.
Among individuals 65 and older the risk of adverse outcomes is higher 12%
Possible Reinfarction
only occurs in 1.3 to 2.6% of patients at 1 year and 7.1% at 4 years.
Quality of life
Identified factors that increase the risk of Major advance cardiac event:
- older age
- hypertension
- smoking
- reduced ejection fraction
- chronic obstructive pulmonary disease
- elevated creatinine
- cancer
- elevated CRP
Requires further investigation that may require longer hospitalizations. It is commonly found that Myocardial Infarctions is missed in women due to non classic presentations such as shortness of breath, dizziness, nausea or unusual fatigue. Patients with MINOCA do present with recurrent chest pains without myocardial infarction.
Literature Cited:
- Tamis‐Holland, J. E., & Jneid, H. (2018). Myocardial Infarction With Nonobstructive Coronary Arteries (MINOCA): It ‘s Time to Face Reality! Journal Of The American Heart Association, 7(13). https://doi.org/10.1161/jaha.118.009635
- Takahashi, J., Onuma, S., Hao, K., Godo, S., Shiroto, T., & Yasuda, S. (2023). Pathophysiology and diagnostic pathway of myocardial infarction with non-obstructive coronary arteries. Journal Of Cardiology, 83(1), 17-24. https://doi.org/10.1016/j.jjcc.2023.07.014
- MINOCA from A to Z – American College of Cardiology. (2022, 5 January). American College Of Cardiology. https://www.acc.org/Latest-in-Cardiology/Articles/2022/01/05/17/41/MINOCA-from-A-to-Z
- Reynolds, H. R., & Smilowitz, N. R. (2022). Myocardial infarction with nonobstructive coronary arteries. Annual Review Of Medicine, 74:171-188. https://doi.org/10.1146/annurev-med-042921-111727
- Yildiz, M., Ashokprabhu, N., Shewale, A., Pico, M., Henry, T. D., Quesada, O. (s. f.). Myocardial infarction with non-obstructive coronary arteries (MINOCA). Frontiers In Cardiovascular Medicine, 9. https://doi.org/10.3389/fcvm.2022.1032436
- Reynolds, H. R., & Smilowitz, N. R. (2022). Myocardial infarction with nonobstructive coronary arteries. Annual Review Of Medicine, 74:171-188. https://doi.org/10.1146/annurev-med-042921-111727
- De Oliveira, L. L. H., Correia, V. M., Nicz, P. F. G., Soares, P. R., & Scudeler, T. L. (s. f.). MINOCA: One size fits all? Probably Not—A review of etiology, investigation, and treatment. Journal Of Clinical Medicine, 11(19), 5497. https://doi.org/10.3390/jcm11195497