By Dr. Salman Arain MD
Challenge #1. Here is the baseline angio. The challenge here is wiring the mid LAD. The wire tip shape needed to cross it is different than the one needed to reach it. Our solution – a dual lumen catheter (Sasuke) in the mid LAD which allows us to secure the D2.
Challenge #2. We wired the D1 to secure it during provisional LAD stenting. There is plaque shift +/- thrombus which shuts down the D1 by the time we have treated the mid LAD. Luckily we still had the wire in place – so in goes the Sasuke again. We were able to guarantee that the wires did not end up behind the stent struts.
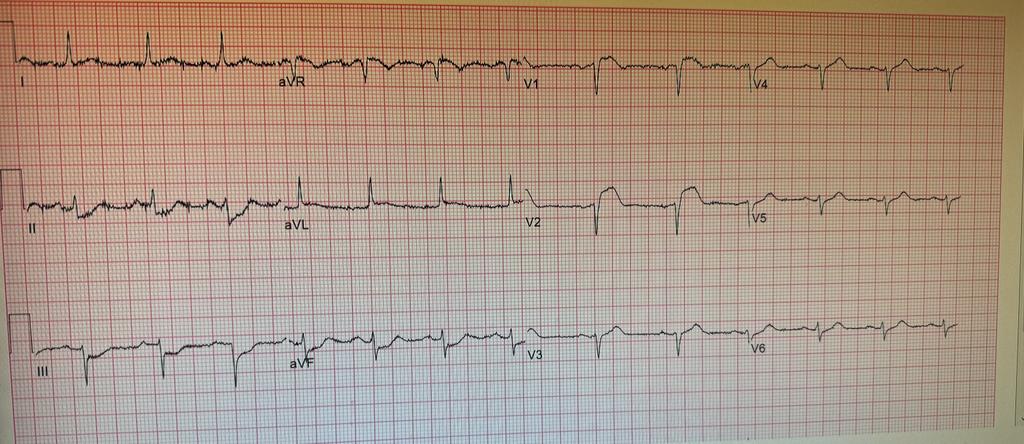
Challenge #3. We did a proximal POT, pulled the jailed wire, and passed it down the LAD. I did not want to keep working on the Fielder. Note the brief detour into D2. Alas, we ended up with a dissection! After this point the patient started vomiting and the ST were really deep. I felt that the 6 Fr guide was workkng against us. As you can see much of the LAD has shut down. Our solution – intubate, insert Impella, upsize to 7 Fr.
Challenge #4. Here is the groin angio through the 14 Fr Impella sheath. The leg will likely become ischemic during the case- so we put in a retrograde SFA sheath for future ‘external bypass’.
Challenge #5. Our first angio after Impella placement shows clot in the entire LAD!!! 😳😩 I called for Penumbra, but decided to make a pass with an Export while the cath lab was setting up. Surprisingly we were able to ‘uncork’ the LAD.
Challenge #6. The next step is to treat the D2 and optimize the mid LAD stent. There is stent recoil. IVUS showed a fibrotic lesion – we treated this with a cutting balloon and completed the LAD PCI. Or did we…
Challenge #7. The completion angio shows thrombus in the proximal LAD – address it with medications or aspirate? We tried PTCA but it embolized. Well, by this time the Penumbra was set up. We were able to complete the procedure (again!). This is the final coronary angio.
Challenge #8 (No more, I promise): How to keep the leg perfused while the Impella was in place? Here is a clip of the initial angio through the Impella sheath. The third clip is through the SFA sheath (using a micropuncture dilator) after the external bypass has been set up (right CFA -> left SFA). I do this to confirm pulsatility in the occluded leg.

This is what the set up looks like. There are several advantages to doing it this way. The retrograde sheath is easier to insert, doesn’t compromise antegrade flow to the leg, allows you to do an angio to confirm Impella sheath closure (if done), perform internal balloon tamponade on the proximal arteriotomy (if needed) and importantly – makes sure there is no dead zone in the CFA. As a bonus, you can close this with an AngioSeal later if needed.
The End.
Question: How would you take out the antegrade sheath? Manual and balloon tamponade the CFA from contralateral?
Answer: They are both retrograde. The angio shows it. It looks antegrade because of the body habitus.
The typical sequence is:
1) Remove Impella
2) Exchange Impella sheath for new sheath without flushing
3) You may do an angio from the lower (SFA) sheath at this stage. This is optional.
4) Treat the proximal arteriotomy with Manta or double Perclose.
5) Confirm closure with injection through the lower sheath.
5a) Consider balloon tamponade from the lower sheath if needed.
6) Close the lower arteriotomy if the SFA is ‘clean’ – you must use a device. It is too deep for manual hemostasis.
7) Confirm close from the contralateral side.
1) These are recommendations for Impella inserted in an emergency – and expected to stay in for some time. Usually there is no time for Preclose if the patient is crashing.
2) Also, I don’t Preclose unless I know the Impella is coming out within 6-12 hours.
2b) We have left the sutures in longer but management becomes an issue if the CCU stay is prolonged.
3) You don’t have to put a new Impella sheath in. Any 14 Fr sheath will do.
4) The idea is that there may be thrombus in the old sheath – in the space between the sheath and the Impella.
4b) Of course, you can hook it up to pressure to keep it open – but we have had thrombus form despite that too.
5) When the Impella comes out, you can use your favorite method to obtain hemostasis. Double Perclose is just one.
6) Stick the SFA in the cleanest part – avoid being too close to the Impella sheath. You don’t want the lower sheath tip ‘tucked under’ the Impella sheath.
We have left Impellas in upto 5 days with good leg perfusion using this method. The best part is that you can take it out yourself in the cath lab. No need for the OR.
Question: SA; trying to understand..
The need for# 6? Why is the SFA stick needed?
This is required when the Impella sheath is occlusive in the iliacs or the CFA. In such cases the leg with the Impella becomes ischemic.
One way to prevent this is to gain antegrade access into the CFA or SFA and create an ‘external bypass’. Usually this is done with US guidance and is a little tricky.
Our method makes it wasy because you can stick the SFA without changing the side you are standing on. Also, if you use a roadmap (like we did) you can do it without US. Because there is usually some flow via the profunda: CIA -> IIA -> PFA -> CFA/SFA.
Question: Also, for the SFA are you using an Arrow sheath ?
Answer: Yes, always an Arrow sheath. Given the depth of the vessel and the angles involved, you need a braided sheath. Non-braided sheaths will typically soften and kink.