By Dr. Salman Arain
85 year old man admitted with CP in setting of HTN. Had has symptoms for a few months. ECG showed ST depression and the EF was 45%. The referring sent him for CABG but the (chief) surgeon was hesitant because the patient is a Jehovah’s witness (can not receive blood), low platelets (85k), and high Cr (1.9)
.
What is your ABC analysis? As a reminder:
A – angiographic analysis,
B – bifurcation strategy,
C – calcium modulation,
D – device (MCS) selection if any, and
E – execution strategy?
Ok, so the resolution of our case…
These were my thoughts going into the case…
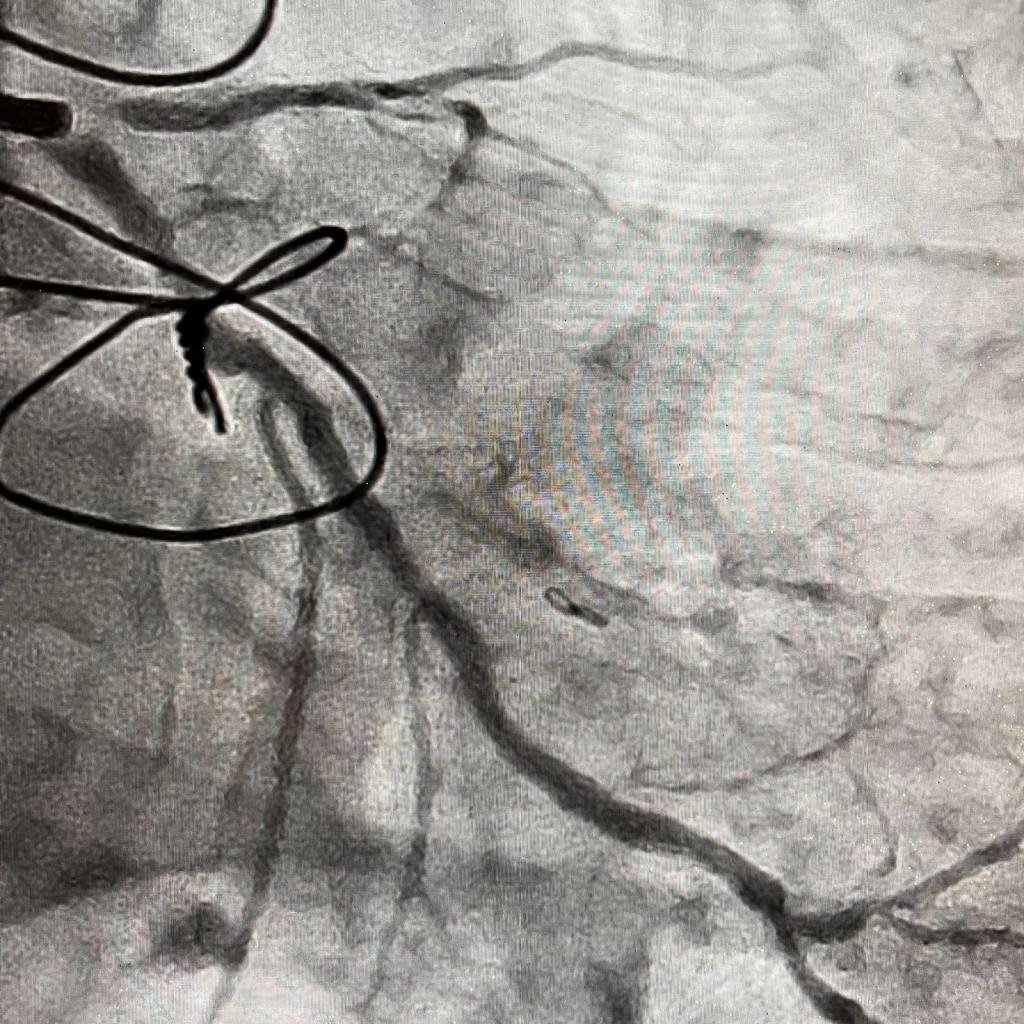
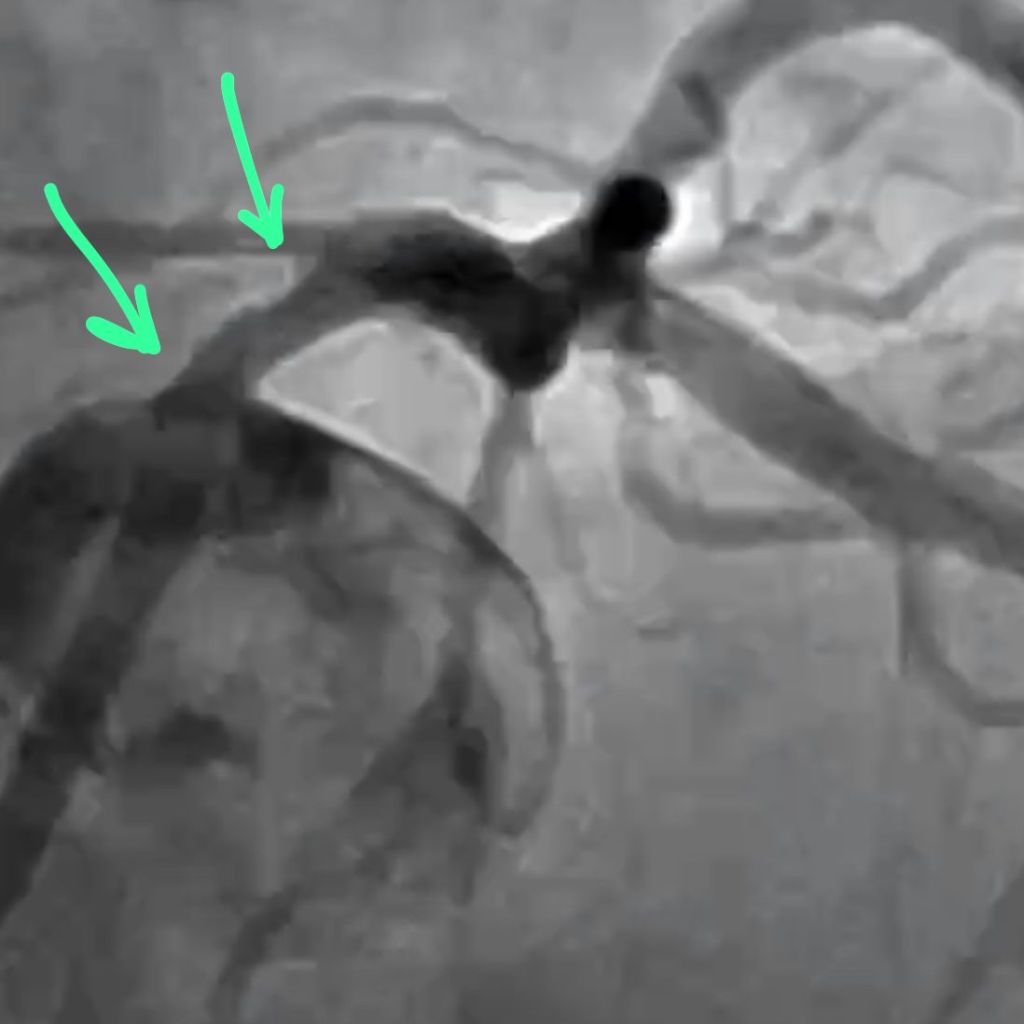
A. Functional last conduit because the RCA is critical. The entire body of the LM is involved. Heavy calcium is an understatement.
B. Medina 1,1,1 – both arteries need to be addressed. Our plan was to perform DK crush.
C. Rota and/or IVL. ‘Relative’ disadvantages to both – Rota will require me to remove the wire from one of the branches. IVL will prolong LM occlusion (= ischemic) time.
D. Definitely Impella supported.
E. Plan – perform RHC for reserve, insert Impella, wire both LAD and LCX, PTCA LM into LAD, IVUS then decide on rota strategy, finish with DK crush. Stage RCA.
We started by doing a RHC. The PA pressures were not too bad (48) and the PA sat was reassuring 58%. We opted for dual access.
We resolved that issue with a TurnPike LP microcatheter. You can drive the MC by torquing it. We knew we were going to fix the LAD with rota so I did a 1.5 mm angioplasty to allow the LAD to breathe while we did IVUS.
With the LAD and LCX fixed, the LM is more manageable now. We opted to finish the T-stent and use IVUS to see if further optimization was needed.Our bifurcation plan rapidly evolved during the case. It was DK crush before the case, mini crush after I put the proximal LCX stent in, and ended up being a T-stent because of how well the stent had landed at the ostium.
You can see the patient is becoming restless. I think that it was likely from leg ischemia related to the Impella sheath.
Also, the guide had softened and came out. Note the stent deformation on account of the calcium module at the ostium. There is a recoil after high-pressure NC ballooning.
Here is the CFA after Impella removal. We did not use single access because I wanted to use a 7 French guide without any of the drama. A 7 French sheath is often quite snug in the Impella insertion sheath. The double access also allowed us to ensure that the bleeding at the Impella insertion site had completely stopped before the patient left the Cath Lab. This was on on account of his inability to receive blood being a Jehovah’s witness.
The patient did very well. He was up and about the next day. He did have a mild bump in his creatinine, but we kept him for a few days.
I plan to perform an PET in four weeks and then decide if he needs the RCA fixed. Again, he is an 85 year old who has been doing quite well until now.
The End. 🙏🏼
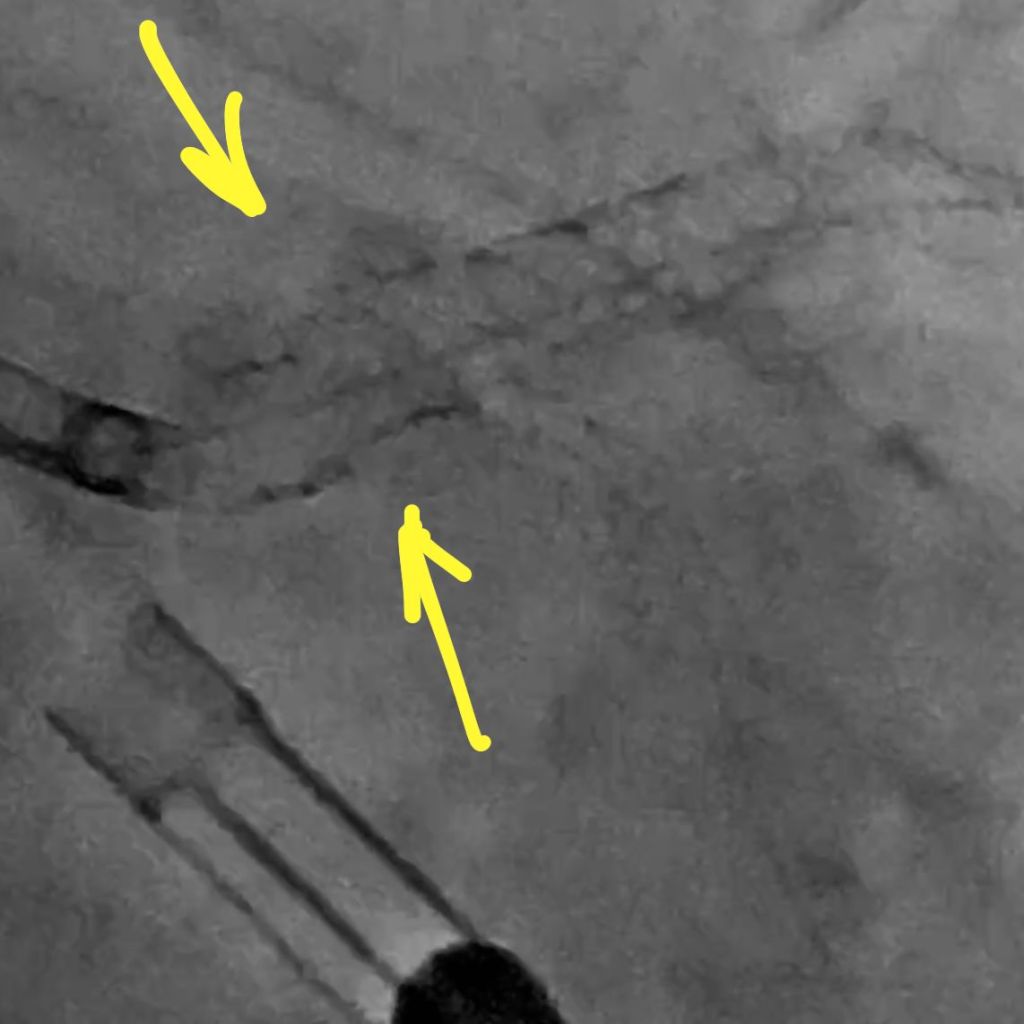
I am going to share a series of still frames that shows the changing morphology of the LM lumen. This is baseline.

Here is the balloon inflation. Note the upward displacement of the nodules.
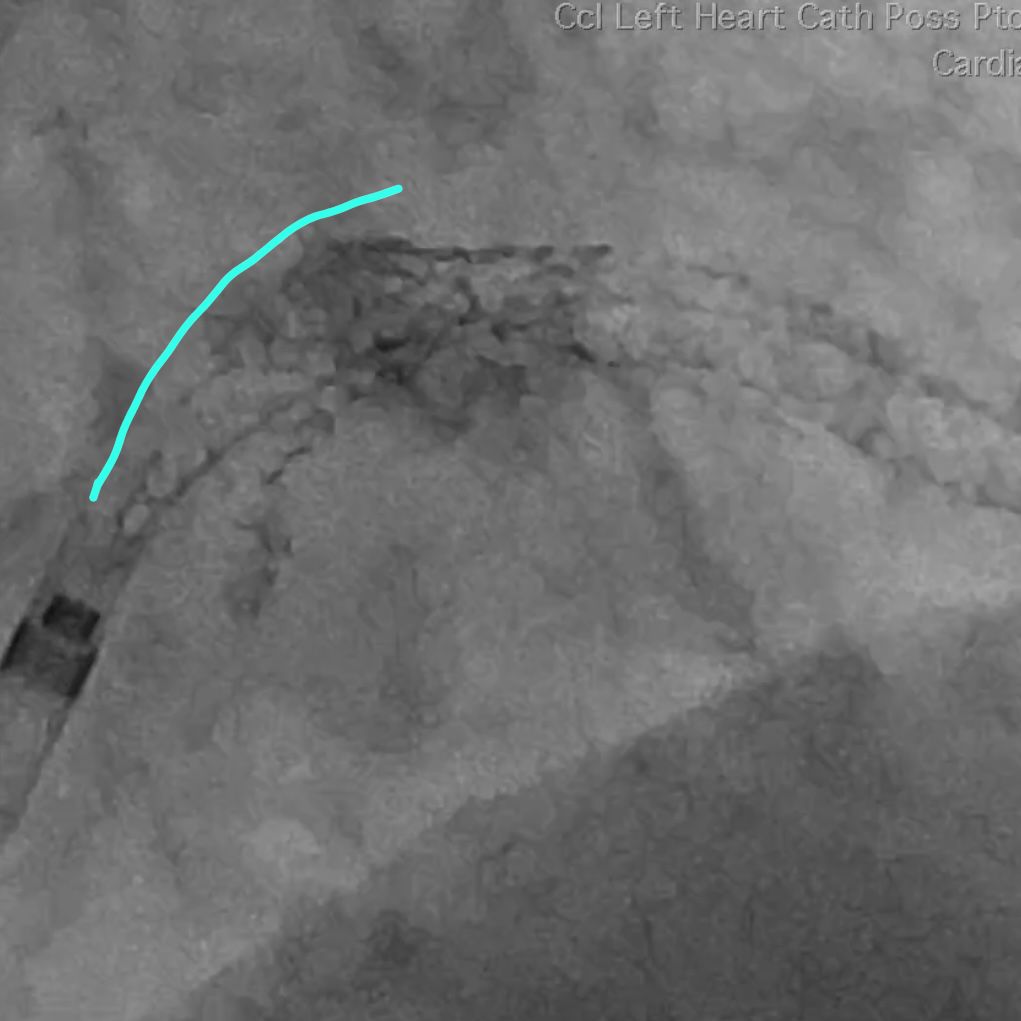
This is after our aggressive POT. Note the smoother upper curvature.