Case Report and Discussion
Hema Manvi Koneru, MBBS
Rajiv Gandhi Institute of Medical Sciences, Telangana, India.
Amanpreet Kaur, MBBS
Government Medical College Patiala, India.
Divyasri Koneru, MBBS
Dr.Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, India
Amin H. Karim MD FACC,
Clinical assistant professor, Baylor College of Medicine, Houston, Texas.
A 74-year-old male presented with complaints of dizziness. His medical history includes hypertension, diabetes mellitus, mitral regurgitation, tricuspid regurgitation, and a transient ischemic attack five months prior. Additionally, he reported two episodes of memory lapses within the past year.
The patient denied experiencing orthopnea, paroxysmal nocturnal dyspnea, chest pain, smoking, shortness of breath, leg swelling, speech disturbances, disequilibrium, blurry vision, syncope, tinnitus, hearing loss, ataxia, numbness, tingling, pins, and needles in the arms or legs.
MEDICATIONS
Aspirin 81mg sustained-release oral tablet, once daily; atorvastatin calcium 80mg tablet, taken orally once daily; clopidogrel 75mg tablet, taken orally daily; dulaglutide 0.75mg/0.5ml subcutaneous pen injector, administered subcutaneously once weekly; gabapentin 300mg oral capsule, taken once daily; losartan 25mg tablet, taken orally once daily; metformin hydrochloride 750mg extended-release tablet, taken twice daily with meals; nitroglycerin 0.4 mg sublingual tablet, to be used when chest pain persists; and thiamine 100 mg oral tablet, taken once daily. These medications have been prescribed to effectively manage the patient’s medical conditions and symptoms.
The patient had a history of allergy to the contrast medium used for the radiological examination.
LAB WORKUP
- HBA1C-6.6gm/dl
- The rest of the blood reports- are within in normal range.
ELECTROCARDIOGRAM
- Sinus tachycardia with nonspecific ST-abnormality
CTA CORONARY ARTERIES
- There is severe coronary calcification. The observed calcium score is 780, which is at the 75th percentile for subjects of the same age, gender, race/ethnicity who are free of clinical cardiovascular disease and treated diabetes.
- Moderate to severe, predominantly calcified. Coronary artery disease involving proximal and LAD with moderate luminal stenosis. FFR-CT was performed on the LAD which showed significant flow limitation of the mid-LAD (left anterior descending artery).
CTA OF BRAIN AND NECK
- Brain–moderate chronic microvascular ischemia, suprasellar 8 x 7 mm partially calcified lipoma or dermoid cyst.
- Neck-Complete occlusion of the left vertebral artery V1 and V2 segments. Atherosclerosis of bilateral extracranial carotid arteries without significant stenosis.
- The head shows no significant stenosis or occlusion.
MRI BRAIN
- No acute ischemia.
- Hypothalamus showing non-enhancing mass suggestive of Lipoma/Dermoid cyst.
- Moderate chronic microvascular ischemia.
ECHOCARDIOGRAM
- Mild left ventricular hypertrophy.
- Trace tricuspid regurgitation.
- Mitral regurgitation.
- Left ventricular dysfunction.
NUCLEAR STRESS TEST
- A small area of perfusion defect in the inferior wall which fills with reperfusion
CAROTID ULTRASOUND
No occlusive disease.
Following a thorough workup and assessment of the patient’s clinical presentation, imaging studies, and diagnostic tests, a final diagnosis of subclavian steal syndrome was made. This condition is attributed to the underlying pathology of atherosclerosis which mainly affects the subclavian artery.
DEFINITION
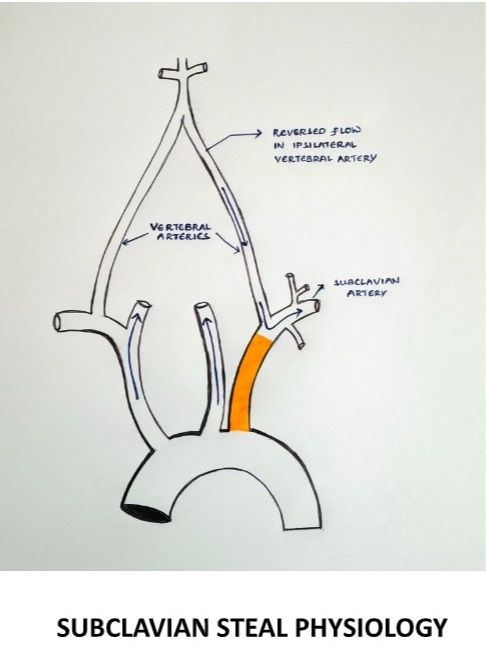
It is characterized by the retrograde flow of blood in the vertebral artery, primarily resulting from significant stenosis or occlusion in the pre-vertebral subclavian artery resulting in cerebrovascular symptoms on the ipsilateral side of the occlusion.
§ During exertion, the subclavian artery steals blood from the vertebrobasilar artery circulation to supply the arm, which leads to vertebrobasilar insufficiency.
SUBCLAVIAN STEAL PHYSIOLOGY
EPIDEMIOLOGY
The prevalence of subclavian steal syndrome has not been well defined, although subclavian steal physiology has been reported in 1.3 to 2.6% of the general population of patients with extracranial atherosclerosis (1,2) as well as within subsets of those presenting with acute ischemic stroke (3)
ETIOLOGY
- The most common cause is atherosclerosis.
- Other vascular causes- Takayasu arteritis, giant cell arteritis
- Arterial thoracic outlet syndrome
- Congenital anomalies- anomalies of the aortic arch, anomalies of the brachiocephalic trunk
- A consequence of corrective surgery- surgical repair of the Tetralogy of Fallot with a Blalock-Taussig anastomosis, surgical management of the coarctation of the aorta.
- Hemodialysis vascular access associated (AV fistula).
Subclavian stenosis more commonly occurs on the left side (>75 percent), possibly due to more acute origin on the left subclavian artery resulting in accelerated atherosclerosis from increased turbulence. (4,5,6)
CLINICAL FEATURES
Neurovascular symptoms can be caused by vertebrobasilar ischemia of the brainstem or cerebellum
- Symptoms include dizziness, vertigo, binocular double vision, dysarthria, syncope, and drop attacks (sudden falls without loss of consciousness) (7)
- Episodes can be precipitated by exercise of the ischemic arm and precipitated by certain head movements.
Atypical neurological presentations- there is also increasing recognition that patients with vertebrobasilar insufficiency can present with other types of symptoms not directly attributable to brainstem or cerebellar ischemia.
- Subarachnoid hemorrhage (8)
- Cognitive and mood abnormalities
EVALUATION
Although neurovascular symptoms associated with subclavian steal physiology occur in only a minority of patients, symptoms of vertebrobasilar ischemia demand critical evaluation (10,11)
When to suspect subclavian steal syndrome
- Diagnosis should be considered in patients with a measurable upper extremity blood pressure differential who develop episodic neurological symptoms attributable to the brainstem or cerebellar ischemia.
- Suspicion is increased if the episodes are provoked by arm exercise, especially if accompanied by ischemic arm symptoms (7)
PHYSICAL EXAMINATION
- All major pulses should be palpated, and blood pressure should be checked in both arms.
- It is important to examine the subclavian arteries in the supraclavicular fossa using palpation and auscultation for paraventricular bruits, also vertebral and carotid arteries for the evidence of any occlusive arterial disease.
- On examination, there may be a significant decrease in the blood pressure on the affected side with a pulse delay appreciated when palpating the radial arteries simultaneously known as RADIO-RADIAL DELAY.
- Check for any evidence of thromboembolism in the skin of the hands and nailbeds of the affected extremities.
- Ischemia affecting the temporo-occipital areas of the cerebral hemispheres or segments of the brainstem and cerebellum characteristically produces bilateral symptoms.
RADIOLOGICAL EXAMINATION
Initial vascular imaging
1. Duplex ultrasound
- A subclavian artery peak systolic velocity >240cm/sec is predictive of a significant (>70 percent) subclavian artery stenosis (9)
- When severe stenosis (>80 percent narrowing) of the proximal subclavian artery is present, 65 percent of pa>ents have permanent flow reversal in the ipsilateral vertebral artery, and 30 percent have intermittent flow reversal (10,11)
2. Transcranial doppler ultrasound
Confirmatory vascular imaging
- Computed tomographic angiography (CTA)-provides precise measurement of the severity of the stenosis. main drawback is the absence of dynamic flow information.
- Magnetic resonance angiography (MRA)- sensitive than CTA. Does not depict images of arterial anatomy but rather the behavior and speed of the flowing protons in the vessel. Also provides information on the intracranial cerebrovascular circulation.
- Catheter-based digital subtraction angiography (DSA)
DIAGNOSIS
DIAGNOSTIC CRITERIA– the presence of subclavian steal physiology with demonstration of a subclavian artery stenosis/ occlusion proximal to the origin of the vertebral artery causing
- Marked reduction in the ipsilateral brachial artery blood pressure.
- Reversal of the direction of blood flow in the ipsilateral vertebral artery
- Neurological symptoms referrable to the vertebrobasilar circulation (cerebellum, brainstem, thalamus, occipital regions)
The likelihood that the presence of subclavian steal physiology will lead to the subclavian steal syndrome increases as the brachial pressure differential between the two limbs becomes more pronounced, particularly >40mmhg (5)
DIFFERENTIAL DIAGNOSIS
These include all the potential causes of vertebrobasilar embolism due to atherosclerosis, hypertension, hypercoagulable states, tumors, tobacco smoking, trauma, and others
MANAGEMENT
Management of patients with subclavian steal syndrome is individualized depending on the etiology, type, and severity of symptoms and their impact on quality of life
ATHEROSCLEROTIC SUBCLAVIAN STEAL SYNDROMEAPPROACH
For most patients with atherosclerosis as the etiology for subclavian steal syndrome, conservative management is the preferred initial therapy.
Initial medical management
- Start with the low-dose aspirin.
- However, the addition of other anti-platelet drugs does not seem justified since this condition is hemodynamic derangement. once a decision is made for surgical management, additional anti-thrombotic agents are required.
- Optimal blood pressure management is required within the ipsilateral side brachial artery.
Surgical management
- Proximal subclavian endarterectomy, which is a trans-thoracic approach used for revascularizing the subclavian artery.
- Re-vascularization surgery via endovascular techniques (carotid-subclavian bypass or subclavian-carotid transposition).
- Carotid intervention in patients with severe concomitant carotid artery disease helps to improve cerebral perfusion.
NON-ATHEROSCLEROTIC SUBCLAVIAN STEAL SYNDROME
- For non-atherosclerotic subclavian syndrome etiologies, the primary cause needs to be addressed.
- Example- Takayasu arteritis is by systemic glucocorticoids or steroid-sparing agents like biological DMARD (Disease Modifying Anti-Rheumatoid Drugs) or non-biological DMARD
CONCLUSION
This case highlights the importance of a detailed evaluation of subclavian steal syndrome can be due to atherosclerosis or non-atherosclerotic causes like Takayasu arteritis, giant cell arteritis, arterial thoracic outlet syndrome, and other causes. In our case, it might be a subclavian steal syndrome secondary to atherosclerosis.
REFERENCES
- Fields WS, Lemak NA. Joint Study of extracranial arterial occlusion. VII. Subclavian steal–a review of 168 cases. JAMA. 1972 Nov 27;222(9):1139-43. PMID: 4678043.
- Hennerici M, Klemm C, Rautenberg W. The subclavian steal phenomenon: a common vascular disorder with rare neurologic deficits. Neurology. 1988 May;38(5):669-73. doi: 10.1212/wnl.38.5.669. PMID: 3362359.
- Bajko Z, Motataianu A, Stoian A, Barcutean L, Andone S, Maier S, Drăghici IA, Cioban A, Balasa R. Prevalence and Clinical Characteristics of Subclavian Steal Phenomenon/Syndrome in Patients with Acute Ischemic Stroke. J Clin Med. 2021 Nov 10;10(22):5237. doi: 10.3390/jcm10225237. PMID: 34830519; PMCID: PMC8621575.
- Ochoa VM, Yeghiazarians Y. Subclavian artery stenosis: a review for the vascular medicine practitioner. Vasc Med. 2011 Feb;16(1):29-34. doi: 10.1177/1358863X10384174. Epub 2010 Nov 15. PMID: 21078767.
- Labropoulos N, Nandivada P, Bekelis K. Prevalence and impact of the subclavian steal syndrome. Ann Surg. 2010 Jul;252(1):166-70. doi: 10.1097/SLA.0b013e3181e3375a. PMID: 20531004.
- Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, McDermott MM. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004 Aug 4;44(3):618-23. doi: 10.1016/j.jacc.2004.04.044. PMID: 15358030.
KESTELOOT H, VANHOUTE O. REVERSED CIRCULATION THROUGH THE VERTEBRAL ARTERY. Acta Cardiol. 1963;18:285-99. PMID: 14045892.
Rodriguez-Lopez JA, Werner A, Martinez R, Torruella LJ, Ray LI, Diethrich EB. Stenting for atherosclerotic occlusive disease of the subclavian artery. Ann Vasc Surg. 1999 May;13(3):254-60. doi: 10.1007/s100169900254. PMID: 10347257.
Gutierrez GR, Mahrer P, Aharonian V, Mansukhani P, Bruss J. Prevalence of subclavian artery stenosis in patients with peripheral vascular disease. Angiology. 2001 Mar;52(3):189-94. doi: 10.1177/000331970105200305. PMID: 11269782.
- Osiro S, Zurada A, Gielecki J, Shoja MM, Tubbs RS, Loukas M. A review of subclavian steal syndrome with clinical correlation. Med Sci Monit. 2012 May;18(5):RA57-63. doi: 10.12659/msm.882721. PMID: 22534720; PMCID: PMC3560638.
- Cornelissen SA, Heye S, Maleux G, Daenens K, van Loon J, De Vleeschouwer S. Treatment of ruptured subclavian steal flow-related vertebrobasilar junction aneurysms: Case report on surgical and endovascular considerations from two cases. Int J Surg Case Rep. 2022 Jan;90:106744. doi: 10.1016/j.ijscr.2021.106744. Epub 2021 Dec 30. PMID: 34991048; PMCID: PMC8741505.
Murumkar V, Jabeen S, Peer S, Ramalingaiah AH, Saini J. Ruptured vertebrobasilar junction aneurysm unmasking subclavian steal syndrome. Surg Neurol Int. 2020 Dec 4;11:419. doi: 10.25259/SNI_561_2020. PMID: 33365182; PMCID: PMC7749953.
Ahuja CK, Joshi M, Mohindra S, Khandelwal N. Vertebrobasilar Junction Aneurysm Associated with Subclavian Steal: Yet another Hemodynamic Cause for Aneurysm Development and Associated Challenges. Neurol India. 2020 May-Jun;68(3):708-709. doi: 10.4103/0028-3886.288981. PMID: 32643699.
Tonetti DA, Jankowitz BT. Subclavian Steal Flow-Related Aneurysm Formation. World Neurosurg. 2019 May;125:101-103. doi: 10.1016/j.wneu.2019.01.186. Epub 2019 Feb 8. PMID: 30743034.
- Mousa AY, Morkous R, Broce M, Yacoub M, Sticco A, Viradia R, Bates MC, AbuRahma AF. Validation of subclavian duplex velocity criteria to grade severity of subclavian artery stenosis. J Vasc Surg. 2017 Jun;65(6):1779-1785. doi: 10.1016/j.jvs.2016.12.098. Epub 2017 Feb 17. PMID: 28222983.
- Nicholls SC, Koutlas TC, Strandness DE. Clinical significance of retrograde flow in the vertebral artery. Ann Vasc Surg. 1991 Jul;5(4):331-6. doi: 10.1007/BF02015293. PMID: 1878290.
- Harper C, Cardullo PA, Weyman AK, Patterson RB. Transcranial Doppler ultrasonography of the basilar artery in patients with retrograde vertebral artery flow. J Vasc Surg. 2008 Oct;48(4):859-64. doi: 10.1016/j.jvs.2008.05.057. Epub 2008 Aug 9. PMID: 18692344.

